
Case Series
Ann Surg Perioper Care. 2023; 8(2): 1059.
Integration of Telemedicine and Hypochlorous Acid Wound Care: A Promising Approach as Illustrated by Four Case Studies
Hendrik C Roos, MD1*; Mazizi Njokweni2; Themba Donovan3; Tebogo Pamela Sedibe, RN4
1Trifectiv (Pty) Ltd, Stellenbosch, South Africa
2Head podiatrist Leratong Tertiary Hospital, Gauteng, South Africa
3Podiatrist, Leratong Tertiary Hospital, Gauteng, South Africa
4Unjani Clinic, Thulamahashe, South Africa
*Corresponding author: HC Roos Trifectiv (Pty) Ltd, Stellenbosch, South Africa. Email: labs@trifectiv.com
Received: July 26, 2023 Accepted: August 21, 2023 Published: August 28, 2023
Abstract
Telemedicine has revolutionized the healthcare industry, providing patients and healthcare professionals with convenient and efficient ways to access and deliver remote healthcare services. One area where telemedicine has shown tremendous promise is in wound care, and in particular, the use of hypochlorous acid (HOCl) as a therapeutic agent. This article aims to explore the benefits of telemedicine in wound care and delve into the specific advantages of employing non-toxic HOCl solution as therapeutic agent. Through case studies, we propose for the integration of telemedicine and non-toxic HOCl wound care, highlighting its potential to improve patient outcomes, enhance accessibility, and reduce healthcare costs.
Keywords: Telemedicine; non-toxic hypochlorous acid; Trifectiv® Plus Wound & Burn Care; Infection; Inflammation; Conservative debridement; Biofilm; Wound care; Wet-to-moist debridement; Gauze dressing
Introduction
Wound care is a complex and resource-intensive aspect of healthcare that demands timely and appropriate treatment to prevent complications and promote optimal healing. Telemedicine, the use of telecommunication technology to provide remote clinical care, has emerged as a valuable tool in delivering wound care services [1]. Through virtual consultations, telemedicine enables healthcare providers to assess wounds, provide expert guidance, and monitor progress remotely [2].
HOCl, a potent antimicrobial, anti-biofilm, and anti-inflammatory agent, has shown efficacy in wound management [3]. Hypochlorous acid is a naturally occurring molecule that occurs in the white blood cells. It is generated by the human immune system in response to infection and injury and plays a crucial role in the eradication of pathogens. Advances in methods to produce medical grade stable HOCl have contributed to its exposure as a wound care treatment agent. Furthermore, its anti-biofilm and anti-inflammatory effects are central in the treatment of chronic wounds [4]. HOCl has also gained attention due to its efficacy against Multiple Drug Resistant (MDR) pathogens, including MDR fungi, whilst not demonstrating any cytotoxicity [5].
A simplified yet effective dressing protocol was developed to treat most wounds, including wounds suitable for home treatment. The dressing consists of surgical non-woven gauze wetted with HOCl (Trifectiv) and placed on the wounds. In the case of cavity wounds, the wetted gauze is plugged into the cavities. The dressings are retained with a crepe bandage or breathable plaster. In the case of lower limb wounds, elastic stockings compliment the treatment protocol, if there are no circulatory restraints to local compression.
Case Study Presentation
Case 1 (Figure 1)
Patient history: A 68-year-old female patient presented to the podiatry clinic of a tertiary health facility with a large open wound on the dorsum of her right foot and ankle. Three weeks prior to presentation, necrotizing fasciitis with surgical debridement resulted in a non-healing wound. Co-morbidities treated on oral medication included metabolic syndrome, diabetes mellitus Type 2, hypertension, and raised serum cholesterol. As the wound was infected and inflamed and exhibited necrotic material, further debridement had been scheduled, with the possibility of below-knee amputation, due to exposed extensor tendons. Prior to the podiatric consultation, the patient had been dressing the wound daily with non-medicated paraffin gauze retained with a crepe bandage. The wound was malodorous and had a pain severity level of 8/10. The wound was not responding to paraffin gauze dressings.
Wound progression (Figure 1): On examination, a wound extended over the anterior aspect of the right ankle and the dorsum of the right foot, sparing the toes. The edges of the wound were inflamed and covered in purulent exudate. After irrigation with non-toxic hypochlorous acid solution (HOCl) 380 mg/L (available as Trifectiv® Plus Wound & Burn Care), the wound was dressed. The dressing consisted of surgical non-woven gauze wetted with HOCl and retained with a crepe bandage. The patient was instructed on the method of dressing to be done daily at home. Follow-up appointments at the clinic were scheduled at weekly intervals. The patient was given contact details for the clinic and for electronic transfer of photographs of the wound twice per week. Sufficient monitoring of the wound required the transmission of photos of the removed dressing as well. The clinic arranged multi-disciplinary referral for the treatment for her co-morbidities.

Figure 1:
Week 3: Infection and inflammation under control which was evident in a reduction in pain, redness around the wound edges, swelling and odour. Conservative wet-to-moist debridement was successful in removing most of the necrotic tissue. Non-viable tendons appeared demarcated.
Week 6: Pain reduced from intensity 8/10 to 6/10. In-clinic sharp debridement removed the remaining necrotic tissue. Wound edges were approximated to reduce the size of the wound. No clinical evidence of infection. No evidence of wound exudate. The patient was referred for plastic surgery and subsequently received a successful skin graft.
Case 2 (Figure 2)
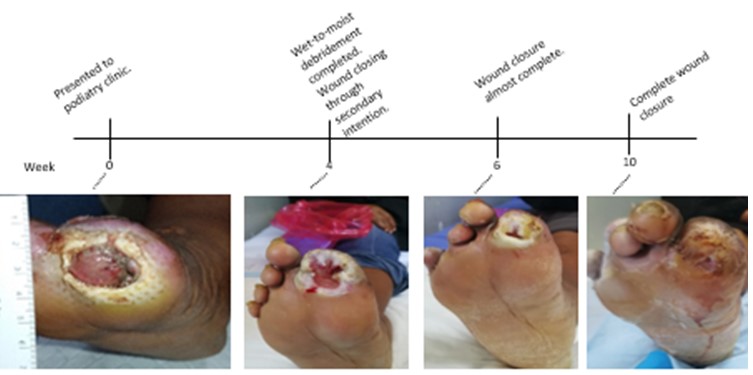
Figure 2:
Patient history: A 62-year-old female Type-2 diabetic patient presented to the podiatry clinic with a Diabetic Fot Ulcer (DFU) on the right foot. The wound, located on the distal phalanx of the first toe, was infected, malodourous, and inflamed, with significant swelling present in the peri-wound area. Extensive wound exudate that appeared as whitish brown discharge was present. The size of the ulcer measured 2x3 cm with the depth of 0,7 cm. Co-morbidities included hypertension and hypothyroidism, for which she was on oral medication.
Previous treatment for six months consisted of antimicrobial silver foam dressings and sterile gauze, retained with a crepe bandage. The patient also received multiple courses of antibiotics.
Wound progression (Figure 2): The foot was washed in lukewarm tap water and dressed in clean non-sterile gauze wetted with non-toxic hypochlorous acid solution 380 mg/L (available as Trifectiv® Plus Wound & Burn Care). The dressing was retained with a crepe bandage. The toe ulcer was plugged with unfolded wetted gauze, ensuring that all parts of the wound was in contact with the wetted gauze. No systemic antibiotics were given. The health care provider instructed the patient the method of daily dressing of his wound. During dressing changes, the patient would electronically send photographs taken of the wound as well as the removed dressing for evaluation by the health care provider. The clinic also arranged for weekly follow-up visits.
By day 4, the patient communicated reduction in malodour, redness, pain, and wound exudate. After one week, the exudate had stopped, and the wound started to close. Daily dressings with hypochlorous acid solution and gauze were continued and by week 4, the wound had reduced to less than half its original size. Complete wound closure was complete by week 10. The patient received instruction on footcare and was referred for orthopaedic footwear, as well as the diabetes clinic for evaluation and blood sugar control.
Case 3
Patient history (Figure 3): Five weeks prior to electronic transmission of photos to the author in South Africa, this 73-year-old female from the Netherlands was involved in a motor vehicle accident in which she sustained extensive soft tissue injuries on the anterior aspect of her right lower leg. Her local health care provider treated her wounds with sharp debridement, povidone iodine, silver impregnated dressings and NSAI gel for pain. Electronic images of her wounds were shared for advice on treatment, as the wound had not shown any healing. On review of the photograph, there was a 10x12 cm wound on the distal aspect of the right lower leg. The peri-wound area was inflamed, and the wound surface was poorly vascularized and had a yellow appearance and was swollen.
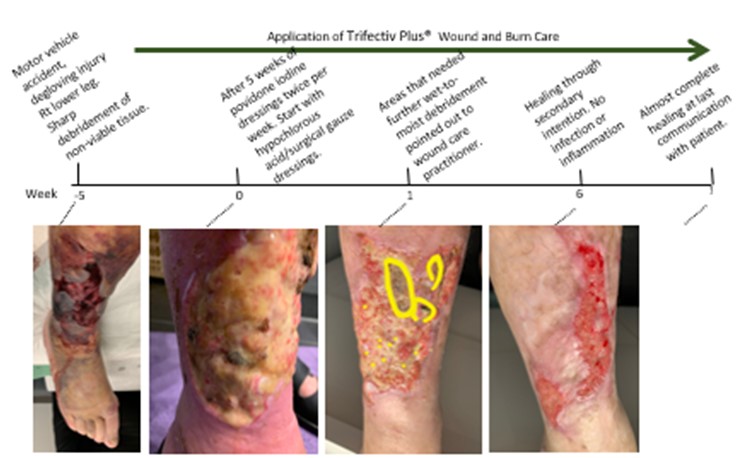
Figure 3:
Wound progression: A wound care protocol consisting of 3 x per week non-toxic hypochlorous acid solution-wetted gauze dressings were suggested to the patient. The patient’s wound care practitioner agreed to apply dressings at home. At the time After the first week of dressings, electronic photograph transmission from the care giver to the patient point specific areas where mechanical debridement could assist in the timeous removal of all necrotic tissue. We recommended that the dressing frequency be increased from 3 x per week to daily dressings. This was to assist the wet-to-moist gauze debridement of necrotic tissue from the wound.
After six weeks of non-toxic hypochlorous acid gauze dressings, the wound appeared to be healing through secondary intention. After eight weeks, the wound was completely healed.
Case 4 (Figure 4)

Figure 4:
Patient history: 50-year-old female presented at a rural secondary healthcare clinic in South Africa with a 11 x 5.5 cm wound on the dorsum of her left foot. The wound was 1.5 cm deep and covered in black material, which had been applied by a traditional healer. The patient complained of severe pain. The foot felt warm with a normal foot pulse. The lower leg was swollen, and a foul odour and puss emanated from the wound and from cavities under the foot. The patient had no co-morbidities.
Wound progression: The foot and lower leg were washed in lukewarm tap water by the health care provider (a registered nurse). The wash did not remove the black material from the wound surface. A dressing consisting of non-sterile clean surgical non-woven gauze, wetted with non-toxic hypochlorous acid solution 380 mg/L was plugged into the dorsal and ventral wounds and retained with a crepe bandage. The patient received a course of penicillin antibiotics and pain medication. The clinic nurse performed the dressings the first seven days. During this time, family of the patient were instructed on the dressing technique, and they were asked to communicate daily via electronic photo transmission of the wound and removed dressings, for evaluation by the clinic nurse.
Conservative wet-to-moist debridement of the foreign substance in the wound and all necrotic material was complete after one week. After a further eleven weeks of daily dressings, wound healing was complete with little scar formation. The patient returned to her normal daily routine.
Discussion
Currently available evidence suggests that telemedicine seems to have similar efficacy and safety and met noninferiority criteria with conventional standard care of chronic wounds [6]. Telemedicine eliminates geographical barriers, enabling patients to receive wound care regardless of their location. It improves access to specialized wound services, particularly for patients residing in remote areas. Telemedicine reduces the need for travel and associated inconveniences, especially in frail patients with affected mobility. It facilitates real-time wound monitoring, allowing for professionals to assess wound progression [7]. Early detection of complications such as infection, inflammation, or delayed healing is possible, enabling timely intervention and optimizing wound care management [8]. By eliminating the need for in-person visits, telemedicine reduces healthcare costs for both patients and healthcare systems. It minimizes travel expenses and potential time off work for patients, while healthcare facilities can optimize their resources by efficiently allocating wound care professionals to virtual consultations. Additionally, telemedicine may decrease the likelihood of hospital readmissions, resulting in further cost savings [9].
Telemedicine also empowers patients to actively participate in their wound care. During the first consultation, the simplified yet effective wound dressing protocol is explained and demonstrated to the patient. This protocol allows for regular dressing changes (5 to 7 times per week), which we found to be more beneficial to wound healing than the common practice of twice weekly or sometimes even once a week dressing changes. In our experience, active involvement in their wound care program promotes adherence to the treatment plan. Patients gain a better understanding of wound management, leading to improved outcomes and reduced healthcare utilization [10].
Hypochlorous acid disrupts microbial membranes and kills biofilm. Biofilm causes inflammation and once a wound is locked in inflammation, it becomes difficult to heal. HOCl is effective against biofilm polysaccharide matrix and the pathogens that produce it. HOCl also has anti-inflammatory properties that accelerates the wound repair process. Non-toxic and non-allergenic, HOCl is safe for use on various wound types and is well-tolerated by patients. It does not induce resistance and does not cause allergic reactions, making it suitable for long-term wound care management [4].
HOCl wound care solutions also promote a moist wound environment, which has been shown to facilitate faster healing, reduce pain, and minimize scarring [11].
Trifectiv Plus Wound & Burn Care (Thoclor Labs, Stellenbosch, South Africa) contains 380 mg/L medical grade stable, non-toxic HOCl solution which has been shown to be beneficial in the treatment of a variety of wounds, including acute and chronic wounds (including MDR-infection), radiation dermatitis, burns infected with biofilm and for the treatment of diabetic foot ulcers and, in cases of healing of large wounds through secondary intent [12].
The components of the HOCl/surgical gauze treatment system are inexpensive, costing less than 50 ZAR (2.50 $US) per dressing. Using a simplified dressing system as described holds many advantages over standard of care more complex dressings and wound treatment systems (e.g., silver impregnated dressings, vacuum treatment system) due to the multi-function (anti-infective, anti-biofilm, anti-inflammatory) qualities of the HOCl as well as the gauze used in the dressing. The gauze serves as vehicle for the delivery of HOCl to all areas of the wound, while it also absorbs wound exudate and conservatively debrides the wound with every dressing change. This type of debridement is called wet-to-moist debridement.
Wet-to-moist wound debridement holds many benefits for telemedicine home care of wounds. It is non-invasive and cost-effective and does not require anaesthesia or an operating room. The gentle debridement of necrotic tissue is performed by the gauze without the need for specialized equipment or extensive resources, reducing healthcare expenses. It is a straightforward technique that can be easily performed by patients [11]. On changing the gauze dressing daily, necrotic tissue including dead biofilm adheres to the gauze and is then removed [13]. There is usually minimal bleeding and trauma associated to wet-to-moist debridement. HOCl-wetted gauze provides a moist environment that helps soften and loosen necrotic tissue, making it easier to remove without causing further damage. This type of debridement is however not suitable for wounds with extensive necrotic tissue. It is important to consult with a healthcare professional to determine the most suitable debridement approach for a particular wound.
Conclusion
Telemedicine and hypochlorous acid wound treatments are two important areas in healthcare that have seen significant growth and development in recent years. Challenges include the availability of technology (e.g., cell phone with quality camera and access to data networks), health provider and patient adoption. Further development include integration with AI and other technologies, which can enhance the capabilities of telemedicine, including machine learning algorithms for diagnosis and treatment monitoring.
While hypochlorous acid has shown promise in wound care, there is still a need for more research to fully understand its full potential and optimal use. There is a lack of standardization and quality control in the production and use of hypochlorous acid solution wound treatments, which can result in variability in its effectiveness and safety. Ongoing research into the development of non-toxic medical grade solution of hypochlorous acid, will facilitate integration with other wound care products.
Author Statements
Conflict of Interest
H Roos, MD: Co-founder of Trifectiv (Pty) Ltd, Stellenbosch, South Africa
References
- Dobke M, Renkielska A, De Neve J, Chao J, Bhavsar D. Telemedicine for problematic wound management: enhancing communication between long-term care, skilled nursing, and home caregivers and a surgical wound specialist. Wounds. 2006; 18: 256-61.
- Carlson T, Collins L. A long distance relationship that works exploring telemedicine in wound care. Today’s wound clinic. 2009; 3: 25-6.
- Armstrong DG, Bohn G, Glat P, Kavros SJ, Kirsner R, Snyder R, et al. Expert recommendations for the use of hypochlorous solution: science and clinical application. Ostomy Wound Manage. 2015; 61: S2-S19.
- Sakarya S, Gunay N, Karakulak M, Ozturk B, Ertugrul B. Hypochlorous acid: an ideal wound care agent with powerful microbicidal, antibiofilm, and wound healing potency. Wounds. 2014; 26: 342-50.
- https://trifectiv.com/mdr-results/.
- Chen L, Cheng L, Gao W, Chen D, Wang C, Ran X. Telemedicine in chronic wound management: systematic review and meta-analysis. JMIR MHealth UHealth. 2020; 8: e15574.
- Haleem A, Javaid M, Singh RP, Suman R. Telemedicine for healthcare: capabilities, features, barriers, and applications. Sens Int. 2021; 2: 100117.
- Nagle SM, Stevens KA, Wilbraham SC. Wound assessment. StatPearls. 2022; 2023.
- Halstead LS, Dang T, Elrod M, Convit RJ, Rosen MJ, Woods S. Teleassessment compared with live assessment of pressure ulcers in a wound clinic: a pilot study. Adv Skin Wound Care. 2003; 16: 91-6.
- Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff (Millwood). 2013; 32: 207-14.
- Junker JP, Kamel RA, Caterson EJ, Eriksson E. Clinical impact upon wound healing and inflammation in moist, wet, and dry environments. Adv Wound Care (New Rochelle). 2013; 2: 348-56.
- https://trifectiv.com/news-articles/page/2/.
- Roos H. The use of hypochlorous acid in the healing of a diabetic foot ulcer. Int J Biomed Eng Clin Sci. 2022; 8: 53-6.