
Case Report
Austin Cardio & Cardiovasc Case Rep. 2023; 8(3): 1061.
Anesthesia Management for Asymptomatic Aortic Narrowing
Walid Atmani*; Ayoub Boubekri; Ilyass Hamadat; Jaafari Abdelhamid; Hicham Balkhi; Mustapha Bensghir
Pole Anesthésie-Réanimation Hôpital Militaire d’Instruction Mohamed V, Rabat, Morocco
*Corresponding author: Walid Atmani Pole Anesthésie-Réanimation Hôpital Militaire d’Instruction Mohamed V Rabat, Morocco. Email: atmani.walid@gmail.com
Received: August 12, 2023 Accepted: September 25, 2023 Published: October 02, 2023
Abstract
An 80-year-old patient admitted to the emergency department for a fracture of the lower extremity of the femur. The clinical examination reveals a stable patient with normal hemodynamic, respiratory, and neurological status. There are no medical history records. The pre-anesthetic evaluation is unremarkable with normal test results. The patient is transported to the operating room, and after spinal anesthesia, experiences hemodynamic instability due to a tight asymptomatic mitral stenosis observed during the clinical examination.
Introduction
Calcified aortic stenosis (AOR) is the most common valve disease indeveloped countries and its prevalence is constantly increasing reaching 2.8% of patients over 75 years old [1], which represents a real public health problem due to the aging of the population [1]. The classic symptoms of severe RAo (angina, dyspnea and syncope) occur at an advanced stage of the disease [2].
In these elderly patients, the diagnosis and care are sometimes delayed. The symptomatology is difficult to assess in patients who are often physically limited, by age and the presence of associated comorbid factors. This population, so-called asymptomatic, is composed, in half of the cases, of patients “False asymptomatic”; it must be unmasked by a stress test if this is possible [3,4] and by the dosage of biomarkers [5,6], in order not to not ignore a low noise RAC which could have benefited from treatment surgical. These little-known patients will progress slowly towards the cardiac decompensation.
The role of the anesthetist is major in the risk assessment either the RA is already known and all elements must be gathered (in particular ETT<6 months-1 year) which will allow the decision to be taken; or the RA is suspected before the discovery of an unknown breath and the first step will be to confirm (or to rule out) the diagnosis by an essential ETT [7].
Observation
An 80-year-old patient was admitted to the emergency department with a fracture of the distal femur. Upon admission, the patient was stable with a Heart Rate (HR) of 80 beats per minute, Blood Pressure (BP) of 12/7 cmHg, and oxygen saturation (SpO2) of 99% on room air.
Clinical Examination
• Cardiac examination: Regular sinus rhythm with no rhythm or conduction disturbances. No murmurs or additional sounds on auscultation.
• Respiratory examination: No crackles, and the patient is stable.
• Neurological examination: The patient is conscious with no focal neurological deficits.
• Additionally, the patient is experiencing pain related to the fracture, showing signs of lower limb trauma.
Upon admission to the emergency department, a preoperative assessment was performed, and analgesics were administered. The pre-anesthetic evaluation determined the patient as ASA 1, an 80-year-old without dyspnea, and a superior functional capacity (4 METs achieved previously). There are no criteria for difficult intubation or ventilation. The patient is deemed suitable for surgery, with a preoperative fasting time of 6 hours.
In the operating room: The patient is positioned on a heated operating table with standard monitoring, including a cardiac scope, 3-lead ECG, pulse oximeter, and non invasive blood pressure monitoring. A fluid resuscitation with normal saline (0.9%) is initiated. The patient is placed in a sitting position for a spinal anesthesia procedure after thorough aseptic preparation. A trocar is introduced at the L4-L5 level, and 12.5 mg of bupivacaine, 25 mcg of fentanyl, and 100 mcg of morphine are injected.
No abnormality
Mild stenosis or sclerosis
Moderate stenosis
Severe stenosis
Other lesion
Murmur heard (n=96)
30(31%)
35(36%)
16(17%)
7(7%)
8(8%)
No Murmur heard (n=278%)
175(63%)
78(28%)
8(3%)
1(0.5%)
16(6%)
Table 1: Presence of a murmur detected by auscultation in relationship to severity of aortic stenosis by echocardiography in hip fracture patients. Values are number (proportion) [9].
After draping by the surgeon, 15 minutes following the spinal anesthesia, the patient presents hemodynamic instability with unmeasurable blood pressure and altered consciousness. This necessitates the placement of a central venous catheter for administration of vasoactive drugs, such as norepinephrine, and conversion to general anesthesia with invasive blood pressure monitoring. The surgical procedure is minimized, and the patient is transferred to the postoperative intensive care unit. After meeting the necessary prerequisites, the patient is extubated with a low dose of vasoactive medication, without any deficits or sequelae.
A postoperative cardiac evaluation with an echocardiogram reveals severe mitral stenosis with an effective valve area of 0.6 cm2, necessitating cardiovascular management. The patient is transferred to the cardiology service for further care.
Discussion
The role of the anesthetist is major in the risk assessment the RA is suspected before the discovery of an unknown breath and the first step will be to confirm (or invalidate) the diagnosis with an essential TTE, the second step of reasoning then being identical to the first case of fig. We must remember the high prevalence of RAC in the octogenarian (>10%) to underline the importance auscultation during the anesthesia consultation, as long as the ACR remains long asymptomatic. The elements to be gathered are: the abolition of B2, the search (sometimes difficult) for stress symptoms, ultrasound criteria severity of ACR, the existence of associated significant mitral insufficiency, marked systolic LV dysfunction (EF <40%). Finally in cases where the stress assessment is impossible or negative, the stress ultrasound may be indicated [7].
The main anaesthetic concern aroused by an undiagnosed heart murmur is the possibility of severe aortic stenosis. This has previously been shown to be a major risk factor for morbidity [8]. Aortic stenosis is increasingly common in our ageing population and its severity increases with age. Before our report, the prevalence and severity of aortic stenosis in an unselected patient population admitted with a surgical diagnosis of hip fracture was unknown. We found that 8% of patients who underwent echocardiography had either moderate or severe stenosis. Since we investigated all patients present when the echocardiography technician was available, our data should reflect the entire population of fractured femur patients [9].
A population-based sample from Finland of 501 people reported echocardiographic findings of moderate to severe aortic valve stenosis in 8.8% of females and 3.6% of males in patients aged 75–86 years [10].
Classically, a loud (grade 4/6), late-peaking systolic murmur radiating to the carotid arteries, a single or paradoxically split second heart sound, and a delayed and diminished carotid upstroke, confirm the presence of severe aortic stenosis. However, physical examination findings are specific but not sensitive for making the diagnosis and determining its severity [11]. In previous work, it is usually only those patients who had a previously undiagnosed systolic murmur that would have undergone pre-operative echocardiography [12]. Our evaluation revealed that 87/278 (31%) of patients without clinically detected murmurs had aortic stenosis. Conversely, in the 96 patients where a murmur was heard, 30 (31%) had a normal echocardiogram. Thus, pre-operative auscultation of a murmur does not necessarily reflect either the presence or the severity of the underlying aortic valve disease. However, if a murmur is heard, then moderate or severe aortic stenosis is 8.5 times more likely [9]. At the end of this assessment, in a multidisciplinary manner, a solution must be proposed. To the patient and his family, taking care to provide information on the risks respective and proposed solutions. Many asymptomatic patients can be operated on for their non-cardiac surgery as a first step provided that the management be optimized (Figure 1) [13- 15].
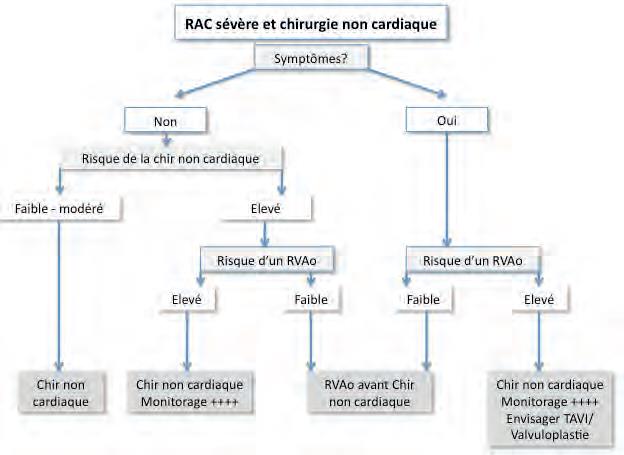
Figure 1: Non cardiac surgery and severe ACR.
Anesthesia and Monitoring [16]
The type of anesthesia (general versus locoregional) matters less than the compliance with the hemodynamic requirements; The essential point remains to avoid any arterial hypotension. So whenever surgery allows it, a trunk or local anesthesia will be preferred. In in other cases most authors recommend general anesthesia; the choice of hypnotic agent and mode of administration (IVD vs TCI) remain to be discuss as long as the monitoring and control of blood pressure is strict. Monitoring the depth of anesthesia allows better titration anesthesia agents. In rare cases preferably for anesthesia perimedullary, sympatholysis should be moderate and progressive; there again the premium blood pressure control. The choice of hemodynamic monitoring is mainly guided by the type surgery and the severity of ACR. The same reasoning applies to the choice of postoperative course. The indication for invasive blood pressure monitoring must be wide. A central venous catheter can be discussed, mainly for administer continuous vasopressor therapy. Transesophageal ultrasound can be used, but requires a trained practitioner. The arterial catheter pulmonary is no longer recommended; there again he assumed a large experience, both in setting up and in interpreting (especially pressures).
Conclusion
Establishing a routine clinical examination seeking for cardiac murmura and echocardiology service can reduce dramatical anesthetic and surgery complications. Although part of this improvement was a function of reduced anaesthetic delay as a result of the echocardiography, other factors also contributed. The evaluation of echocardiography result led to a change in anaesthetic practice, as well as targeting invasive monitoring and increasing clinicians’ vigilance.
References
- Osnabrugge RLJ, Mylotte D, Head SJ, Van Mieghem NM, Nkomo VT, LeReun CM, et al. Aortic stenosis in the elderly: disease prevalence and number of candidates for transcatheter aortic valve replacement: a meta-analysis and modeling study. J Am Coll Cardiol. 2013; 62: 1002-12.
- Ross J, Braunwald E. Aortic stenosis. Circulation. 1968; 38: 61-7.
- AMATO MC, MOFFA PJ, WERNER KE, Ramires JA. Treatment decision in asymptomatic aortic valve stenosis: role of exercise testing. Heart. 2001; 86: 381-6.
- LANCELLOTTI P, KARSERA D, TUMMINELLO G, Lebois F, Piérard LA. Determinants of an abnormal response to exercise in patients with asymptomatic valvular aortic stenosis. Eur J Echocardiogr. 2008; 9: 338-43.
- VAN PELT NC, KERR AJ, Legget ME, Pasupati S, Whalley G, Wong S, et al. Increased B type natriuretic peptide is associated with an abnormal blood pressure response to exercise in asymptomatic aortic stenosis. Int J Cardiol. 2008; 127: 313-20.
- PELTONEN TO, TASKINEN P, SOINI Y, Rysä J, Ronkainen J, Ohtonen P, et al. Distinct downregulation of C type natriuretic peptide system in human aortic valve stenosis. Circulation. 2007; 116: 1283-9.
- Loxdale SJ, Sneyd JR, Donovan A, Werrett G, Viira DJ. The role of routine preoperative bedside echocardiography in detecting aortic stenosis in patients with a hip fracture. Anaesthesia. 2012; 67: 51-4.
- National confidential enquiry into perioperative deaths. Changing the way we operate. The 2001 report of the national confidential enquiry into perioperative deaths. London: NCEPOD, 2001.
- Loxdale SJ, Sneyd JR, Donovan A, G. Werrett1 and D.J. Viira1The role of routine preoperative bedside echocardiography in detecting aortic stenosis in patients with a hip fracture. Anaesthesia. 2012; 67: 51-54.
- Iivanainen AM, Lindroos M, Tilvis R, Heikkilä J, Kupari M. Natural history of aortic valve stenosis of varying severity in the elderly. Am J Cardiol. 1996; 78: 97-101.
- Munt B, Legget ME, Kraft CD, Miyake-Hull CY, Fujioka M, Otto CM. Physical examination in valvular aortic stenosis: correlation with stenosis severity and prediction of clinical outcome. Am Heart J. 1999; 137: 298-306.
- McBrien ME, Heyburn G, Stevenson M, McDonald S, Johnston NJ, Elliott JR, et al. Previously undiagnosed aortic stenosis revealed by auscultation in the hip fracture population-echocardiographic findings, management and outcome. Anaesthesia. 2009; 64: 863-70.
- Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC), European Association for Cardio-Thoracic Surgery (EACTS), Vahanian A, Alfieri O, Andreotti F, Antunes MJ et al. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J. 2012; 33: 2451-96.
- Kristensen SD, Knuuti J, Saraste A, Anker S, Bøtker HE, Hert SD, et al. ESC/ESA Guidelines on noncardiac surgery: cardiovascular assessment and management: the Joint Task Force on noncardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur Heart J. 2014; 35: 2383-431.
- Osnabrugge RL, Kappetein AP, Serruys PW. Non-cardiac surgery in patients with severe aortic stenosis: time to revise the guidelines? Eur Heart J. 2014; 35: 2346-8.
- Mascitti P, Hamdaoui I, Berroëta C, Seince P-F, Montandrau O, Philip I. Rétrécissement aortique et prise. En: Charge péri-opératoire MAPAR. 42 Boulevard Jourdan: Département d’Anesthésie, Institut Mutualiste Montsouris, Paris 14ème. 2017.