
Research Article
Austin J Endocrinol Diabetes. 2023; 10(1): 1098.
A Comparative Study of Plasma N-Terminal Pro- Brain Natriuretic Peptide to Assess Asymptomatic Cardiovascular Disease in Type 2 Diabetic Patients
Sudhir Bhandari1*; Govind Rankawat2; Abhishek Agarwal3; Vishal Gupta4
1Vice Chancellor RUHS Jaipur and Professor Emeritus, SMS Medical College, India
2Assistant Professor, Department of General Medicine, SMS Medical College, India
3Senior Professor, Department of General Medicine, SMS Medical College, India
4Professor, Department of General Medicine, SMS Medical College, India
*Corresponding author: Sudhir Bhandari Vice Chancellor RUHS Jaipur and Professor Emeritus, SMS Medical College, D 126-A, Bapu nagar, Krishna Marg, University Road, Jaipur 302015, India. Tel: 9829078844 Email: drs_bhandari@yahoo.com
Received: April 01, 2023 Accepted: May 12, 2023 Published: May 19, 2023
Abstract
Background: This study aimed to assess NT-pro BNP level in patients of T2DM without overt cardiovascular disease to determine presence of Asymptomatic Left Ventricular Dysfunction (ALVD) compared with matched control group.
Methods: This study conducted at SMS Hospital, Jaipur by selecting 60 patients of type 2 diabetes mellitus and 60 control of non-diabetic population. Information regarding demographic data, clinical symptoms, past medical history, laboratory parameters, NT pro-BNP and 2D Echocardiography collected from selected sample population for comparative analysis among both groups.
Results: Patients of T2DM have significantly higher value of NT pro-BNP, blood sugar and HbA1c with proportionally increased diastolic dysfunction as compared to matched non-diabetic population (P<0.05). Absolute value of NT pro-BNP in patients of T2DM is directly correlated with age, duration of diabetes, Blood pressure, blood sugar level, HbA1c level, creatinine, total cholesterol and urine protein (positive correlation coefficient with P-value<0.05). Left ventricular ejection fractions were found statistically similar among both groups.
Conclusion: Heart failure in patients with T2DM is a most crucial diabetic complication for diagnosis as well as management. Level of NT-pro BNP in blood stream is an important tool for early diagnosis of heart failure especially HFpEF. This study suggests that the secretion of NT-pro BNP is increased in patients with T2DM compared with control subject without overt heart disease. Therefore, measurement of NT-pro BNP paired might be a simple screening tool to identify patients with diabetes at risk for ventricular dysfunction requiring further examination with echocardiography.
Keywords: Diabetes mellitus; Diastolic dysfunction; Echocardiography; HFpEF; NT pro-BNP
Introduction
Diabetes Mellitus (DM) is one of the most challenging public health problems in the 21st century. There is an urgency for greater action to improve diabetes outcomes and reduce the global burden of diabetes now affecting more than 425 million people, of which one-third are people older than 65 years. The estimates of children and adolescents below age 19 with type 1 diabetes have risen to over a million [1]. If nothing is done, the number of people with diabetes may rise to 693 million in 2045, although positively the incidence has started to drop in some high-income countries [2]. At the same time, a further 352 million people with impaired glucose tolerance are at high risk of developing diabetes. By the end of this year, 4 million deaths will happen as a result of diabetes and its complications [3].
Alongside other non-communicable diseases, diabetes is increasing most markedly in the cities of low and middle- income countries. The IDF South-East Asia and Western Pacific regions are at the epicenter of the diabetes crisis: China alone has 121 million people with diabetes and India has a total of 74 million populations with diabetes. African, Middle Eastern, Northern African and South-East Asian regions are expected to face the highest upsurge in the next 28 years. People from these regions develop the disease earlier, get sicker and die sooner than their counterparts in wealthier nations [4].
It is important to know about the awareness level of a disease condition in a population, which plays a vital role in future development, early detection and prevention of disease. Prevention is important because the burden of diabetes and its complications on health care and its economic implications are enormous, especially for a developing country like India. Patient education is always considered an essential element of DM management [5].
Diabetes Mellitus (DM) is a chronic metabolic disorder being characterized by increased blood sugar levels. It is like a termite that insidiously eats up one’s own body and, if not controlled, it cripples the body irreversibly. People get tagged with this incurable disease, if not detected and controlled in earlier stages. Over time, poor glycemic control can lead to multiple chronic complications like damage to eyes (leading to blindness), kidneys (leading to renal failure) and nerves (leading to numbness in the limbs, impotence and foot disorders/possibly amputation) as well as increased risk of heart diseases and stroke [6]. These complications contribute to the decreased quality of life for affected individuals and their families, with a devastating long-term effect on their financial and social wellbeing.
The management of DM largely depends on the affected person’s ability to pursue self-care in daily living. Proper management requires patients to be aware of the nature of the disease, its risk factors, treatment and complications. Thus, effective DM education, with consequent improvements in knowledge, attitudes and skills, leads to better control of the disease and reduce the incidence of complications. Various studies have been conducted in India to look for awareness among diabetics. The Indian Council of Medical Research (ICMR) conducted a study in four regions of India in which they found that only 43.2% of the overall study population had heard about a condition called diabetes [7]. Another study found that 17% of their participants had poor knowledge and more than half believe it to be a communicable disease. Having complete knowledge about the disease is like a small investment for the large benefit [8].
Another major weapon in the management of diabetes is treatment adherence. The World Health Organization (WHO) defined adherence as “the extent to which a person’s behavior – taking medication, following a diet and/or executing lifestyle changes, corresponds with agreed recommendations from a health care provider” [9]. It has been indicated through various studies that despite the extensive therapy options available for various stages of type 2 diabetes, less than 50% of patients achieve the glycemic goals recommended by the American Diabetes Association (ADA) [10,11].
As diabetes is concerned, the knowledge, attitude and practice are dependent on socioeconomic background, habits and cultural beliefs. Proper knowledge of diabetes mellitus can prevent the occurrence of chronic complications associated with DM, which significantly influence the quality of life of patients with diabetes [12]. Diabetes and heart failure are closely related, When the two diseases are considered individually, heart failure has a much poorer prognosis than diabetes mellitus; therefore, heart failure has to be a priority for treatment in patients presenting with the two conditions [13]. It has been estimated that the proportion of CHF patients with known T2DM is 20–35 % [14].
As cardiac dysfunction increases, the synthesis and release of cardiac natriuretic peptides gradually rise in concert with the other neurohormonal responses observed in heart failure. Therefore, it has been proposed that increased B-type Natriuretic Peptide (BNP) and/or N-terminal pro-BNP (NT-pro BNP) be used as a marker for symptomatic ventricular dysfunction. In addition, irrespective of the degree of left ventricular dysfunction, blood BNP or NT- pro BNP levels are elevated in patients with many cardiac disorders, including previous myocardial infarction, cardiomyopathy, valvular heart disease, hypertensive heart disease, and atrial fibrillation [15].
The Framingham study demonstrated that subjects with higher plasma BNP levels exhibited an increased incidence of Congestive Heart Failure (CHF) [16]. It is therefore, possible that BNP or NT-pro BNP levels may serve as a useful marker of cardiovascular risk in the screening of the general population [17]. However, recent reports have shown that in the general population, the plasma BNP or NT-pro BNP level is affected by many extracardiac factors including age, obesity, and genetics [18,19]. Non-invasive cardiac imaging like 2D Echocardiogram and MRI of the heart is essential for diagnosis, evaluation and management of heart failure, but these are time- consuming and less acceptable. However, circulating NT-pro BNP is highly sensitive for Heart Failure with preserved and depressed ejection fraction in the asymptomatic patients. Therefore, elevated NT-pro BNP level may serve as an important diagnostic marker for Heart Failure in patients of T2DM if found to be useful.
Methods
Study Design
This is observational cross-sectional and comparative study, conducted at S.M.S. Medical College and attached Hospital, Jaipur, India from April 2019 to May 2020. This study was approved by the Institutional Ethics Committee. In this study 60 patients of T2DM selected as cases after application of exclusion criteria (patients of severe illness, past history of cardiovascular disorder, chronic lung disease and chronic kidney disease were excluded from this study) and 60 non-diabetic subjects selected as control. The study group underwent detail demographic analysis, clinical manifestation, medical history, treatment history, laboratory investigation especially HbA1c, hemogram, fasting and post-prandial sugar, renal function, urine routine and microscopic examination, NT-pro BNP, ultrasonography abdomen for renal size and 2D-echocardiogram. The data obtained were collected, tabulated, compiled, interpreted and analyzed. Both of these Groups were matched for age, gender and presence of other comorbidities.
Data Collection
All patients of T2DM (HbA1c ≥6.5%) as a cases and healthy subjects of without diabetes mellitus (HbA1c ≤5.5%) selected as control. Selected groups undergo detailed medical history to exclude confounding factors especially past history of cardiovascular disorder, chronic lung disease and chronic kidney disease. Demographic data obtained in the form age, sex, geographic distribution with clinical manifestations and duration of T2DM and other associated comorbidities. Vitals of both groups including systolic and diastolic blood pressure, heart rate and temperature were measured by standard protocol. In blood investigations haemoglobin, Total leukocyte count, Platelet count, fasting and postprandial blood sugar (2 hour after meal), HbA1c, NT pro- BNP, kidney function test, liver function test, total cholesterol and triglyceride were measured in both groups. NT-pro BNP was analyzed using a competitive enzyme immunosorbent assay designed to measure the immunoreactive NT-pro BNP (Biomedica Laboratories, Vienna, Austria). Blood samples were drawn in EDTA tube, immediately placed on ice, and promptly centrifuged at 4°C. NT-pro BNP measurements were done using an ELISA: a two steps sandwich assay with streptavidin coated microtiter plates. This assay does not require sample extraction and there is no detectable cross reactivity with ANP, NT-pro ANP, BNP, or urodilatin. Urine for routine and microscopy and electrocardiograph was examined in both groups. 2D Echocardiography with especial focus on diastolic dysfunction and left ventricular ejection fraction was performed in both groups. Transthoracic echocardiography was performed using a Philips IE 33 machine (Phillips Medical Systems, Best, and The Netherlands). All patients were examined with conventional 2-D and Doppler modalities, combined with color tissue Doppler imaging. Data were stored on compact discs and analyzed off-line with commercially available software (EchoPAC software) by an experienced investigator, with no other relation to the present study and blinded to all other information. The case and control selection were mentioned in (Figure 1).
Statistical analysis
The descriptive statistics for quantitative data was expressed as mean and standard deviation and qualitative data was expressed as proportions. The parameters were compared among different Groups using chi-square and z-score test for significant differences. The level of significance was assigned at a p-value less than 0.05.
Results
A total of 60 patients of T2DM (Group A) and 60 subjects (Group B) of control group selected for study at SMS Medical College and attached group of Hospital, Jaipur, Rajasthan. All necessary data were collected, evaluated, interpreted and correlated within both groups to assess different manifestations of T2DM. Value of NT-pro BNP in patients of T2DM also correlated with various demographic, clinical and laboratory parameters.
Demographic Data (Table 1)
Type 2 DM and Control group
Characteristics
Group 1 Type 2 DM (N=60)
Group 2 Control (N=60)
P- Value
Age (Year)
56.70±6.36
55.73±6.04
0.977
Sex ratio (Female to Male)
0.58
0.62
0.849
Duration of hypertension (year)
2.63±4.67
2.46±4.05
0.832
Personal Habits
Alcoholics
5 (8.33%)
4 (6.67%)
0.726
Smoker
8 (13.33%)
10 (16.67%)
0.610
Alcohol and smoker
7 (11.67%)
8 (13.33%)
0.779
Systolic Blood Pressure (mm of Hg)
131.46±9.85
129.8±9.06
0.338
Diastolic Blood Pressure (mm of Hg)
83.53±7.45
83.86±7.46
0.808
Pulse rate (Per minute)
78.77 ±9.75
80.00±9.14
0.476
Temperature(F)
97.75±0.77
97.56±0.64
0.161
Haemoglobin (g/dL)
12.29±1.35
12.46±1.29
0.473
TLC (x103/μL)
7.18±1.88
7.16±1.78
0.968
Platelets (x Lac/μL)
2.28±0.31
2.34±0.33
0.29
Fasting blood sugar (mg/dL)
143.68±34.45
92.17±10.99
<0.001
PP- blood sugar (mg/dL)
203.38±62.54
123.52±13.79
<0.001
HbA1c (%)
8.08±1.48
5.76±0.53
<0.001
NT-pro BNP (pg/mL)
761.23±787.36
323.5±85.71
<0.001
Urea (mg/dL)
35.22±10.83
30.53±7.49
0.006
Creatinine (mg/dL)
1.23±0.39
0.97±0.28
<0.001
SGOT (U/L)
37.87±12.82
36.53±10.79
0.538
SGPT (U/L)
39.85±13.73
38.33±11.38
0.511
Triglyceride (mg/dL)
181.56±73.44
169.25±32.76
0.238
Total cholesterol (mg/dL)
295.97±92.14
219.55±35.46
<0.001
Urine protein
1.37±0.5
1.13±0.35
0.0024
Ejection fraction by 2D Echo (%)
53.9±2.6
54±2.4
0.827
NT-pro BNP greater than UNL
39 (65%)
37 (61.67%)
0.704
LAD in ECG
11 (18.33%)
9 (15.00%)
0.489
Diastolic Dysfunction in 2D-Echo
13 (21.67%)
4 (6.67%)
0.0182
Table 1: A comparative analysis of patients of T2DM and non-diabetic control group (Quantitative data expressed as mean±SD while qualitative data expressed as numbers with percentage).
The overall mean age of patients of T2DM was 56.7 year (56.70±6.36) and mean age of control group was 55.73 year (55.73±6.04), which had no any statistically significant difference (p=0.977). Sex ratio (female to male) for patients of T2DM were found to be 0.58 while it was 0.62 for control group without any statistically significant difference (p=0.849). In this study, 20 patients (33.33%) had personal history of smoking and/or alcohol in group of T2DM while 22 patients (36.67%) had personal history of smoking and/or alcohol in control group without any statistically significant difference (p=0.704).
General Physical Examination (Table 1)
In this study all patients have average built and nourishment. The mean pulse rate in patients of T2DM were found to be 78.77/minute (78.77±9.75) and in control group were 80.00/minute (80±9.14) (p=0.476). The mean temperature in patients of T2DM were found to be 97.75 of (97.75±0.77) and in control group were 97.56 of (97.56±0.64) (p=0.161). Similarly, no significant difference was observed in blood pressure among both groups.
Laboratory Investigations (Table 1):
All patients of study groups go through base line investigations with special focus on diabetes, renal and cardiac parameters. The mean haemoglobin level was 12.29 g/dL (12.29±1.35) in patients of T2DM and 12.46g/dL (12.46±1.29) in control group (p=0.473). The mean total leukocyte counts were 7.18x103/μL (7.18±1.88) in patients of T2DM and 7.16x103/μL (7.16±1.78) in control group (p=0.968). The mean platelet counts were 2.28lac/μL (2.28±0.31) for patients of T2DM and 2.34lac/μL (2.34±0.33) for control group (p= 0.290). The mean fasting blood sugar of patients of T2DM were found to be 143.68mg/L (143.638±34.45) and for control group were found to be 92.17mg/dL (92.17±10.99) which have statistically significant difference (p<0.001). Postprandial blood sugar also checked just two hours after eating food. The mean post prandial blood sugar was found to be 203.38mg/dL (203.38±62.54) in patients of T2DM and 123.52mg/dL (123.52±13.79) in control group (p<0.001). Blood level of sugar in last three months, a direct reflection of sugar control was estimated by HbA1c in all patients and found that mean value of HbA1c in patients of T2DM was 8.08% (8.058±1.48) and in control group was 5.76% (5.76±0.53) which have statistically significant difference (p<0.001).
NT-pro BNP released from heart as a consequence of increased load on myocardium and supposed to be an indirect reflection of reduced functional capacity of heart. In our study the mean NT-pro BNP for patients of T2DM was 761.23pg/ mL (761.23±787.36) and for control group 323.50pg/mL (323.50±85.71) which have statistically significant difference (p<0.001). Absolute value of NT-pro BNP in patients of T2DM also varied widely which ranges from a minimum value of 70pg/mL to maximum value of 3540pg/mL and 95% CI of 761.23±199.22. The proportion of individuals with a NT-pro BNP value above the cut off value (300pg/mL) was higher (65% vs. 61.67%) among the diabetic patients than in the control group, but not statistically significant (p=0.704). Patients of T2DM had higher mean value of serum urea (35.22mg/dL) as compared to control group (30.53mg/dL) with p=0.006. The mean value of creatinine in patients of T2DM was found to be 1.23mg/dL (1.23±0.39) and in control group it was 0.97mg/dL (0.97±0.28) (p<0.001). The liver function in both groups have no any significant difference.
Lipid profile of two groups were measured by serum level of triglyceride and total cholesterol. In this study the mean value of total cholesterol found to be significantly higher in patients of T2DM (295.97mg/dL±92.14) as compared to control group (219.55mg/dL±35.46) (p<0.001). Renal function in study groups also estimated by urinary protein excretion. In this study the mean value of excreted urinary protein was found to be significantly higher (+1.37) in patients of T2DM as compared to control group (+1.125) (p=0.0024). All patients of study groups also gone through 2D echocardiography to screen for ejection fraction, Left Ventricular Diastolic Dysfunction (LVDD) and other structural or functional disorders. The mean value of ejection fraction in patients of T2DM was found to be 53.9% (53.9±2.6) and in control group it was found to be 54% (54±2.4) without any statistically significant difference (p=0.827). The proportion of patients who had LVDD were found to be 21.67% in group of T2DM while this proportion is significantly lower (6.67%) in control group (p=0.0182).
Impact of laboratory parameters on NT-pro BNP in patients of T2DM (Table 2 & Graph 1)
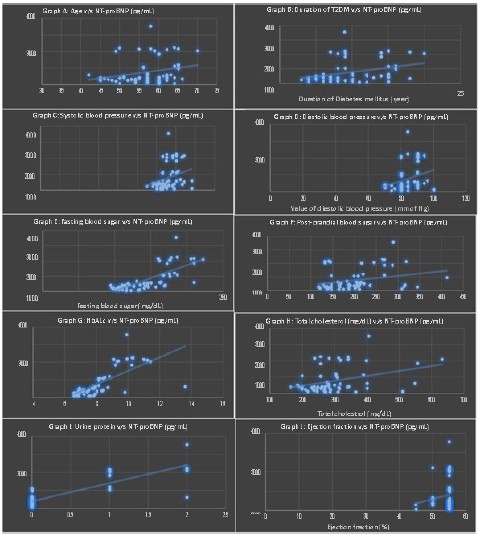
Figure 1: Correlation of NT pro-BNP with (A) Age of patients, (B) Duration of T2DM, (C) Systolic Blood pressure, (D) Diastolic blood pressure, (E) Fasting blood sugar, (F) Postprandial blood sugar, (G) HbA1c, (F) Total cholesterol, Urine protein, (G) Ejection fraction in selected patients of T2DM.
Characteristics
Correlation Coefficient ‘r’
P value
Age and NT-pro BNP
0.2567
0.047 (S)
Duration of Diabetes and NT-pro BNP
0.3293
0.010 (S)
Systolic Blood Pressure and NT-pro BNP
0.279
0.0308 (S)
Diastolic Blood Pressure and NT-pro BNP
0.3004
0.0196 (S)
Hemoglobin and NT-pro BNP
-0.1454
0.268 (NS)
Blood Sugar (F) and NT-pro BNP
0.7475
<0.001 (S)
Blood Sugar (PP) and NT-pro BNP
0.2628
0.0424 (S)
HbA1c and NT-pro BNP
0.7255
<0.001 (S)
Creatinine and NT-pro BNP
0.5069
0.003 (S)
Total Cholesterol and NT-pro BNP
0.3546
0.005 (S)
Triglyceride and NT-pro BNP
-0.027
0.837 (NS)
Urine Protein and NT-pro BNP
0.848
<0.001 (S)
Ejection Fraction and NT-pro BNP
0.133
0.311 (NS)
Table 2: Correlation of NT pro-BNP with various quantitative data of selected patients of T2DM.
In this study, absolute value of NT-pro BNP in patients of T2DM group also corelated with demographic parameter, chronic medical disease, and laboratory and imaging parameters. In this study, absolute value of NT-pro BNP raised with age of patients with ‘r’ value of +0.2567 (p=0.047). NT-pro BNP also have significant positive correlation with duration of diabetes in patients of T2DM (‘r’=+0.3293, p=0.010). Absolute value of NT-pro BNP also closely related with systolic and diastolic blood pressure of patients of T2DM (value of ‘r’=+0.279, p=0.0308 for systolic blood pressure and NT-pro BNP while value of ‘r’=+0.3004 p=0.0196 for diastolic blood pressure and NT-pro BNP). Absolute value of NT-pro BNP has positive correlation with fasting blood sugar (‘r’=+0.7475, p<0.001) and post prandial blood sugar (‘r’=+0.2628, p=0.0424). NT-pro BNP also raised with value of HbA1c as both have positive correlation with ‘r’=+0.7255 and p<0.001.
In this study, absolute value of NT-pro BNP also positively correlated with serum level of creatinine (‘r’=+0.5069, p=0.003) and serum level of total cholesterol (‘r’=+0.3546, p=0.005) while negative correlation exhibited with triglyceride level (‘r’=-0.027, p=0.837). NT-pro BNP also positively correlated with excreted urinary protein (‘r’=+0.848, p<0.001) and cardiac ejection fraction and NT-pro BNP (‘r’=+0.133, p=0.311).
Discussion
The incidence and prevalence of T2DM increases worldwide. The reasons for this increase are complex but they include: increasing incidence of T1DM in children, especially younger children; increasing incidence of T2DM in young people and increasing incidence of T2DM in adults as a result of sedentary living, high-energy dietary intakes and other as yet unknown factors; the intergenerational effects of hyperglycemia in pregnancy and the general ageing of the global population. On the other hand, earlier diagnosis of T2DM and better management of all types of diabetes leading to greater life-expectancy are also contributing to this rise in prevalence.
Diabetes mellitus is a heterogeneous disease. It is well known from clinical practice that the cardiovascular risk of individual diabetes patients varies widely. Therefore, it seems possible that only certain subpopulations are at risk for the development of cardiac diseases [20]. Heart failure is a major health issue and a risk factor for early death and disability in type 2 diabetes. This study was therefore done at the SMS medical college and attached hospital, Jaipur, in order to assess whether NT-pro BNP has potential role for early detection of heart failure in patients of T2DM.
In this study nearly half of patients are in their sixth decades (51 to 60 year) of life in both groups. In order to avoid age as a confounding factor, mean age in both groups are statistically similar. Male populations are predominant involving 63.33% in group A of diabetic patients and 61.67% in group B of non-diabetic. Gender ratio also statistically similar in both groups to avoid confounding. As per personal addiction like smoking and/or alcohol are considered than both groups have similar prevalence. Both groups have statistically similar vital parameters including pulse rate, temperature, systolic and diastolic blood pressure. All patients of study groups go through base line investigations with special focus on diabetes, renal and cardiac parameters. In patients of T2DM mean value of hemoglobin, total leukocyte counts and platelet counts were found to be within normal range without any specific deviation in absolute value. Both groups have statistically similar value of hemoglobin, total leukocyte counts, platelet counts.
The mean fasting blood sugar (143.68mg/dL) and post prandial blood sugar (203.38mg/dL) were found to be significantly higher in patients of T2DM as compare to control group. Higher value of blood sugar in patients of T2DM has been responsible for precipitations of diabetes related complication especially micro vascular, macrovascular and cardiac complications including heart failure. Similarly, HbA1c in patients of T2DM was found to be significantly higher as compared to control group.
BNP has been shown to be elevated in early left ventricular systolic as well as in diastolic dysfunction [21]. NT- pro BNP is a split product from the BNP. It is more stable, and the circulating concentration is not dependent on the receptor population in the individual patient. In this study, the NT-pro BNP level was shown to be significantly elevated in the cohort of patients with T2DM. Hence, patients of T2DM are more prone to develop cardiac failure as compare to matched non-diabetic person as detected by higher NT-pro BNP level in patients of T2DM. In this study serum level of urea and creatinine also higher significantly in patients of T2DM as compared to control group, which might be confound for NT-pro BNP.
Patients of T2DM also have higher value of total cholesterol as compared to control group while no significant difference was observed for value of triglyceride. Blood lipids of traditional risk value differed between groups as expected, with diabetic patients having higher total cholesterol than control subjects. In addition to the risk of having diabetes, this gives an increased risk of having coronary atherosclerosis. Higher value of cholesterol predisposed for insulin resistance which further aggravate hyperglycemia in patients of T2DM and have higher prediction for heart failure.
Both groups have similar liver function measured by SGOT and SGPT which deny state of acute hepatitis. However, patients of T2DM might have Non-Alcoholic Fatty Liver (NAFLD) which was not detected in this study. The causative mechanism driving NAFLD progression in T2DM and evaluating the results of newer antidiabetic treatments and identification of additional novel targets require future research [22].
In this study random urine sample also withdrawal to detect excretion of urinary protein and found that excretion of protein in urine significantly higher in patients of T2DM as compared to control group. Proteinuria a microvascular complication which reflect diabetic nephropathy in patients of T2DM. V Mohan et al in their study [23] suggest that the frequency of proteinuria was assessed in a cohort of 1848 diabetic patients attending a diabetes center in south India. A total of 127 (6.9%) patients had evidence of macroproteinuria and 49 (2.5%) patients had microproteinuria. Thus overall, 9.4% of patients had diabetes related proteinuria. In addition, 70 patients (3.8%) had evidence of proteinuria with no evidence of retinopathy. The frequency of both microproteinuria and macroproteinuria increased linearly with duration of diabetes. Multiple logistic regression analysis showed that duration of diabetes, serum creatinine, and glycated hemoglobin was risk factors for macroproteinuria.
Heart failure is one of the major cardiovascular complications in patients with Type 2 Diabetes Mellitus (T2DM) and increases the risk of morbidity and mortality. In this study the mean value of ejection fraction in patients of T2DM was found to be 53.9% and in control group it was found to be 54% without any statistically significant difference (p=0.827). The proportion of patients who had LVDD were found to be 21.67% in group of T2DM while this proportion is significantly lower (6.67%) in control group (p=0.0182). Hence, Left Ventricular Failure (LVF) or heart failure with reduced ejection fraction (HFrEF) could not be significantly differ in patients of T2DM and non-diabetic group. So 2D echocardiography does not significantly rely on heart failure status in patients of T2DM. However, proportion of patients having LVDD (HFpEF) were found to be significantly higher in patients with T2DM as compared to non-diabetic control group.
Iwakura K [24] in their study suggest that both heart failure with reduced ejection fraction and that with preserved ejection fraction (HFpEF) is observed in T2DM patients, and HFpEF is often overlooked and misdiagnosed in these population. Left ventricular hypertrophy, left atrial dilatation, diastolic dysfunction, and subclinical systolic dysfunction indicated as reduced global longitudinal strain are major abnormalities on echocardiography in patients with diabetic cardiomyopathy. These structural and functional changes are also prevalent in the general patients with T2DM, and those with these abnormalities have higher incidence of heart failure than those without them. Glycemic control might improve some of these abnormalities on echocardiography, but it is still unclear whether their improvement could be associated with risk reduction for heart failure. Although active management for heart failure is needed in patients with T2DM, traditional treatment and some new class of antihyperglycemic drugs, such as glucagon-like peptide-1 receptor agonists or dipeptidyl peptidase-4 inhibitors, could not reduce the risk of heart failure. Recent major trials demonstrated Sodium–Glucose co-transporter-2 (SGLT2) inhibitors improve prognosis of T2DM patients through prevention of heart failure. At now, there are only limited data on the effects of DPP-4 inhibitors or SGLT2 inhibitors on echocardiography in T2DM patients. Large-scale trials are needed to clarify how antihyperglycemic drugs affect echocardiographic parameters.
In this study absolute value of NT-pro BNP continuously increased with age of patients in T2DM as maximum value of NT-pro BNP was observed in patients of more than 60 year of age. This might be explanation of higher prevalence of heart failure (HFrEF or HFpEF) in advancing age. A linear regression model for age as an independent and NT-pro BNP as a dependent variable suggests an age-related increase in NT-pro BNP. However absolute cut off value for NT-pro BNP also varied as per age of patients as suggested by Bernstein LH [25] the median NT-pro BNP for patients under 50 years is 60.5pg/ml with an upper limit of 462pg/ml, and for patients over 50 years the median was 272.8pg/ml with an upper limit of 998.2pg/ml.
NT-pro BNP have significant positive correlation with duration of diabetes in patients of T2DM (p=0.010). Longer duration of diabetes precipitate for vascular complication and long-term sequel of cardiac dysfunction. Patients of longer duration of diabetes must be closely monitored for heart failure by measuring NT-pro BNP at regular basis. Absolute value of NT-pro BNP also influenced by blood pressure of patients, in this study mean value of NT-pro BNP have positive correlation with both systolic and diastolic blood pressure. Patients with combined T2DM and hypertension are more prone to develop heart failure as compared to isolated T2DM. Miguel Rivera et al suggest [26] that hypertensive patients have higher NT-pro BNP levels than subjects with normal blood pressure. The heart pressure of patients with metabolic abnormalities increases as systolic pressure rises, causing changes in ventricular volume and increased ventricular wall stiffness, leading to increases in ventricular muscle subjected to stretch or wall pressure and increased concentrations of BNP. Diastolic blood pressure may reflect the influence of pulse pressure, as increased pulse pressure (reduced arterial compliance) is likely to be accompanied by lower diastolic blood pressure [27].
The mean value of NT-pro BNP has positive correlation with fasting blood sugar (p<0.001), post prandial blood sugar (p=0.0424) and HbA1c (p<0.001). Hyperglycemic state responsible for increased vascular complication and heart failure in patients of T2DM. It is well known that glucose level is directly linked to CVD risk. A prospective observational study (UKPDS-35) revealed that every 1% reduction in baseline HbA1c levels decreases the incidence of myocardial infarction by 5% [28]. Additionally, as symptomatic hospitalized patients experience physiological and psychological stress, which may increase blood glucose levels. David Aguilar in their study suggest that [29] in a large national cohort of patients with diabetes and established HF, we demonstrate that the association between levels of HbA1C and mortality appears U-shaped, with increased risk of death at both higher and lower HbA1C levels when compared to modest glucose control (7.1%<HbA1C≤7.8). It is estimated that approximately 5 million individuals with HF in the US have co-existing diabetes. It confirms that significantly elevated HbA1C is associated with increased risk in this population and efforts should be made to treat these patients with proven HF therapies and consider glucose lowering therapy. Kursat Dal et al in their study [30] suggest that a significant decrease in BNP (95.0[4.0–1807] ng/L vs. 52.0[2.1–987.0] ng/L, p<0.001) levels were observed, after improving glycaemic control.
In this study NT-pro BNP have positive correlation with serum level of creatinine or impaired renal function test. Patients of T2DM are more prone to develop diabetic nephropathy as a long-term microvascular complication. However, mean value of creatinine were found to be within normal range in patients of T2DM and non-diabetic group both. Blood level of NT-pro BNP were found to be have positive correlation with total cholesterol level while negative correlation with triglyceride level. Deposition of fatty tissue might be responsible for increase insulin resistance in patients of T2DM, which furthermore aggravate hyperglycaemia and heart failure. Wen hua zhu in their study suggest that [31] that there was little association or even a negative association between NT-pro BNP level and waist circumference, triglycerides, low-density lipoprotein and high-density lipoprotein. In addition, dyslipidaemia may cause vascular endothelial cell injury, leading to an increase in neutral endopeptidase release, thus increasing the degradation of BNP [32].
NT-pro BNP also have positive correlation with excreted urinary protein in patients of T2DM. Hulya Taskapan et al [33] provide evidence of an association between NT-pro BNP and proteinuria in type II diabetic patients with macroalbuminuria. Patients with high NT-pro BNP may have more tubular injury. In this study no any significant correlation was noted between NT-pro BNP and cardiac ejection fraction in 2D echocardiogram. However, diastolic dysfunction was found to be higher in patients of T2DM with raised NT-pro BNP. Henrik Reinhard et al [34] showed that among asymptomatic type 2 diabetic patients with microalbuminuria that received intensive multifactorial treatment, patients with increased NT-pro BNP levels did not have more echocardiographic abnormalities. The pathogenesis of LV diastolic dysfunction is not known in detail, but a contribution of increased afterload, e.g. due to augmented arterial stiffness and microvascular disease, reduced myocardial perfusion, and increased myocardial stiffness associated with extracellular matrix alterations, fibrosis and metabolic derangements have been suggested [35]. Interestingly, LV diastolic dysfunction was not related to LV mass or carotid compliance in patients with or without significant CAD, but a strong association with glycemic control (HbA1c levels) was found.
Conclusion
Heart failure in patients with T2DM is a most crucial diabetic complication for diagnosis as well as management. 2D echocardiography is an effective modality to detect heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF). Level of NT-pro BNP in blood stream also an important tool for early diagnosis of heart failure especially HFpEF. This study suggests that the secretions of NT-pro BNP is increased in patients with T2DM compared with control subject without overt heart disease. Therefore, measurement of NT-pro BNP paired might be a simple screening tool to identify patients with diabetes at risk for ventricular dysfunction requiring further examination with echocardiography.
Author Statements
Ethical Approval
This study proved by ethical and research committee of SMS medical college and Hospital, Jaipur, India.
Author Contributions
S. Bhandari, G. Rankawat and A. Agrawal formulated the research questions, designed the study, developed the preliminary search strategy, and drafted the manuscript; G. Rankawat and V. Gupta collected and analyzed data for study. G. Rankawat wrote the manuscript. S. Bhandari and A. Agrawal conducted the quality assessment. All authors critically reviewed the manuscript for relevant intellectual content. All authors have read and approved the final version of the manuscript.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not for profit sectors.
Availability of Data and Materials
Available from corresponding author upon reasonable request.
Declaration of Competing Interest
All authors report no potential conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential.
References
- Foma MA, Saidu Y, Omoleke SA, Jafali J. Awareness of diabetes mellitus among diabetic patients in the Gambia: a strong case for health education and promotion. BMC Public Health. 2013; 13; 1124.
- World Health Organization, Global Report on Diabetes. Geneva, 2016. 2018.
- Mafomekong A, Yauba S, Semeeh A, James J. Awareness of diabetes mellitus among diabetic patients in the Gambia: a strong case for health education and promotion. BMC Public Health. 2013; 13: 1124.
- International Diabetes Federation. Available at: http:// www.idf.org /membership/sea/india
- Diabetes can be controlled in 80 percent of Cases in India. IANS. news. biharprabha.com. 2014.
- Deepa M, Bhansali A, Anjana RM, Pradeepa R, Joshi SR, et al. Knowledge and awareness of diabetes in urban and rural India: The Indian Council of Medical Research India Diabetes Study (Phase I): Indian Council of Medical Research India Diabetes 4. Indian J Endocrinol Metab. 2014; 18: 379–85.
- Desai R, Vadgama P, Parth D. Effect of awareness of diabetes on clinical outcomes of diabetes: an observational study at a private hospital in Gujarat. National journal of medical research. 2012; 2: 493-96.
- World Health Organization. Adherence to Long-Term Therapies. Evidence for Action. Geneva: World Health Organization; 2003. Available at: http://whqlibdoc.who.int /publications/2003/9241545992.pdf. 2013.
- Bailey CJ, Kodack M. Patient adherence to medication requirements for therapy of type 2 diabetes. Int J Clin Pract. 2011; 65: 314–22.
- Morisky 8-item medication adherence questionnaire. http://www.uk.stage.cecentral.com/assets/9544/MMAS8_-_UNTHSC.pdf.
- Latifeh A, Reem S. Awareness and knowledge about Diabetes Mellitus among Students at Al – Balqa Applied University: Pakistan Journal of Nutrition. 2012; 11: 1023-8.
- Demaio AR, Otgontuya D, de Courten M, Bygbjerg IC, Enkhtuya P, et al. Exploring knowledge, attitudes and practices related to diabetes in Mongolia: a national population-based survey. BMC Public Health. 2013; 13: 236.
- Rani PK, Raman R, Subramani S, Perumal G, Kumaramanickavel G, et al. Knowledge of diabetes and diabetic retinopathy among rural populations in India, and the influence of knowledge of diabetic retinopathy on attitude and practice. Rural Remote Health. 2008; 8: 838.
- Tsutamoto T, Wada A, Maeda K, Hisanaga T, Maeda Y, et al. Attenuation of compensation of endogenous cardiac natriuretic peptide system in chronic heart failure: prognostic role of plasma brain natriuretic peptide concentration in patients with chronic symptomatic left ventricular dysfunction. Circulation. 1997; 96: 509-16.
- Cowie MR, Struthers AD, Wood DA, Coats AJ, Thompson SG, et al. Value of natriuretic peptides in assessment of patients with possible new heart failure in primary care. Lancet. 1997; 350: 1349-53.
- Dao Q, Krishnaswamy P, Kazanegra R, Harrison A, Amirnovin R, et al. Utility of B-type natriuretic peptide in the diagnosis of congestive heart failure in an urgentcare setting. J Am Coll Cardiol. 2001; 37: 379-85.
- Maisel AS, Krishnaswamy P, Nowak RM, McCord J, Hollander JE, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002; 347: 161-7.
- Yoo BS, Kim WJ, Jung HS, Kim JY, Lee SW, et al. The clinical experiences of B-type natriuretic peptide blood concentrations for diagnosis in congestive heart failure: the single hospital experience based on the large clinical database. Korean Circ J. 2004; 34: 684-92.
- Sutton TM, Stewart RA, Gerber IL, West TM, Richards AM, et al. Plasma natriuretic peptide levels increase with symptoms and severity of mitral regurgitation. J Am Coll Cardiol. 2003; 41: 2280-7.
- Buse JB, Ginsberg HN, Bakris GL, Clark NG, Costa F, et al. Primary prevention of cardiovascular diseases in people with diabetes mellitus: a scientific statement from the American Heart Association and the American Diabetes Association. Diabetes Care. 2007; 30: 162–72.
- Yu CM, Sanderson JE, Shum IO, Chan S, Yeung LY, et al. Diastolic dysfunction and natriuretic peptides in systolic heart failure: higher ANP and BNP levels are associated with the restrictive filling pattern. Eur Heart J. 1996; 17: 1694–1702.
- Dharmalingam Mala, P Ganavi Yamasandhi. Nonalcoholic Fatty Liver Disease and Type 2 Diabetes Mellitus. Indian journal of endocrinology and metabolism. 2018; 22: 421-428.
- Mohan V, Meera R, Premalatha G, Deepa R, Miranda P, et al. Frequency of proteinuria in type 2 diabetes mellitus seen at a diabetes centre in southern India. Postgraduate Medical Journal. 2000; 76: 569-573.
- Iwakura K. Heart failure in patients with type 2 diabetes mellitus: assessment with echocardiography and effects of antihyperglycemic treatments. J Echocardiogr. 2019; 17: 177-186.
- Bernstein LH, Zions MY, Alam ME, Haq SA, Heitner JF, et al. What is the best approximation of reference normal for NT- pro BNP. Clinical levels for enhanced assessment of NT-pro BNP (CLEAN). JMLD. 2011; 2: 16- 21.
- Rivera M, Taléns-Visconti R, Salvador A, Bertomeu V, Miró V, et al. [NT-pro BNP levels and hypertension. Their importance in the diagnosis of heart failure]. Rev Esp Cardiol. 2004; 57: 396-402.
- Wang TJ, Larson MG, Keyes MJ, Levy D, Benjamin EJ, et al. Association of plasma natriuretic peptide levels with metabolic risk factors in ambulatory individuals. Circulation. 2007; 115: 1345–53.
- Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000; 321: 405–412.
- Aguilar D, Bozkurt B, Ramasubbu K, Deswal A. Relationship of hemoglobin A1C and mortality in heart failure patients with diabetes. Journal of the American College of Cardiology. 2009; 54: 422-8.
- Dal K, Ata N, Yavuz B, Sen O, Deveci OS, et al. The relationship between glycemic control and BNP levels in diabetic patients. Cardiology journal. 2014; 21: 252-6.
- Zhu WH, Chen LY, Dai HL, Chen JH, Chen Y, et al. Correlation between B type natriuretic peptide and metabolic risk factors. Archives of medical science: AMS. 2016; 12: 334-40.
- Yu HJ, Jin MJ, Li J, Wang J. Effects of dyslipidemia on plasma brain natriuretic peptide levels of type 2 diabetics. Chin J Diabetes. 2011; 19: 358–60.
- Taskapan H, Taskapan MC, Orman I, Ulutas O, Yigit A, et al. NGAL and NT-pro BNP levels in diabetic patients with macroproteinuria. Renal Failure. 2013; 35: 1273-1277.
- Reinhard H, Hansen PR, Wiinberg N, Kjaer A, Petersen CL, et al. NT-pro BNP, echocardiographic abnormalities and subclinical coronary artery disease in high-risk type 2 diabetic patients. Cardiovasc Diabetol. 2012; 11: 19.
- Boudina S, Abel ED. Diabetic cardiomyopathy revisited. Circulation. 2007; 115: 3213-3223.