
Case Report
Austin J Endocrinol Diabetes. 2023; 10(1): 1100.
Endometrioma Detected on Recombinant TSH-Stimulated 18F-FDG-PET/CT
Tamayo-Carabaño D*; Martínez-Diher L
Department of Nuclear Medicine, Universitary Hospital Fundación Jiménez Díaz, Spain
*Corresponding author: Tamayo-Carabaño Daniella. Department of Nuclear Medicine, Universitary Hospital Fundación Jiménez Díaz, Avda. de los Reyes Católicos, 2, 28040 Madrid, Spain. Tel: +34 915504898 Email: dratamayoc@gmail.com
Received: July 17, 2023 Accepted: August 15, 2023 Published: August 22, 2023
Abstract
A 43-year-old female patient diagnosed with high-grade follicular thyroid neoplasm in October 2022, treated with total thyroidectomy + left laterocervical lymphadenectomy in February 2023 with stage T4N0M0. A study with 18F-FDG PET/CT stimulated with Recombinant Thyroid-Stimulating Hormone (rTSH) was requested prior to performing ablative treatment with radioactive iodine (131I) on the same day. Two days prior to the PET/CT study, a subcutaneous injection of rTSH (Thyrogen®) was administered, presenting, immediately after, pain in the right iliac fossa that did not subside with anti-inflammatories. The PET/CT image shows tumor remains in the anterior cervical region and a pelvic mass dependent on the right adnexa, not previously known, of a cystic nature, septated with FDG uptake, with an SUVmax of 15,3, which partially compresses the ipsilateral ureter. Treatment with 131I was postponed due to acute abdominal pain and it was decided to take him to the operating room where an oopherectomy + right adnexectomy was performed with an anatomopathological result of endometrioid cystadenoma. Due to structural similarities and cross-reactivity between hormones, and the presence of TSH receptors in endometrioid tissue, we propose that the growth of the tumor lesion in this case was precipitated by rTSH administration.
Keywords: 18F-FDG PET/CT; Endometrioma; Recombinant thyroid-stimulating hormone; rTSH; TSH receptors; Thyrogen®
Case Presentation
We present the case of a 43-year-old female patient diagnosed with high-grade follicular thyroid neoplasm in October 2022, who was treated with total thyroidectomy and left laterocervical lymphadenectomy in February 2023 with stage T4N0M0. It was decided to perform ablation of thyroid remnants with radioactive iodine (131I), previously requesting an extension study with 18F-FDG PET/CT the same day. The treatment preparation with 131I would be stimulated with Recombinant Thyroid-Stimulating Hormone (rTSH) administered two days before a daily subcutaneous injection of rTSH (Thyrogen®), which would be used to perform the PET/CT study under the same stimulation.
Immediately after the administration of the injections, the patient began with acute pain in the right iliac fossa that did not subside with anti-inflammatories, and radiated to the ipsilateral flank with positive fist percussion.
The acquisition of the 18F-FDG PET/CT study was performed, showing hyper-uptake foci in the anterior cervical region compatible with thyroid remnants; and a pelvic mass of 9 cm in diameter, dependent on the right adnexus, not previously known, of a cystic nature, septated, with FDG uptake, with an SUVmax of 15,3, partially compressing the ipsilateral ureter. These findings are reported as a pelvic mass suggestive of malignancy given its morphometabolic characteristics (Figure 1).
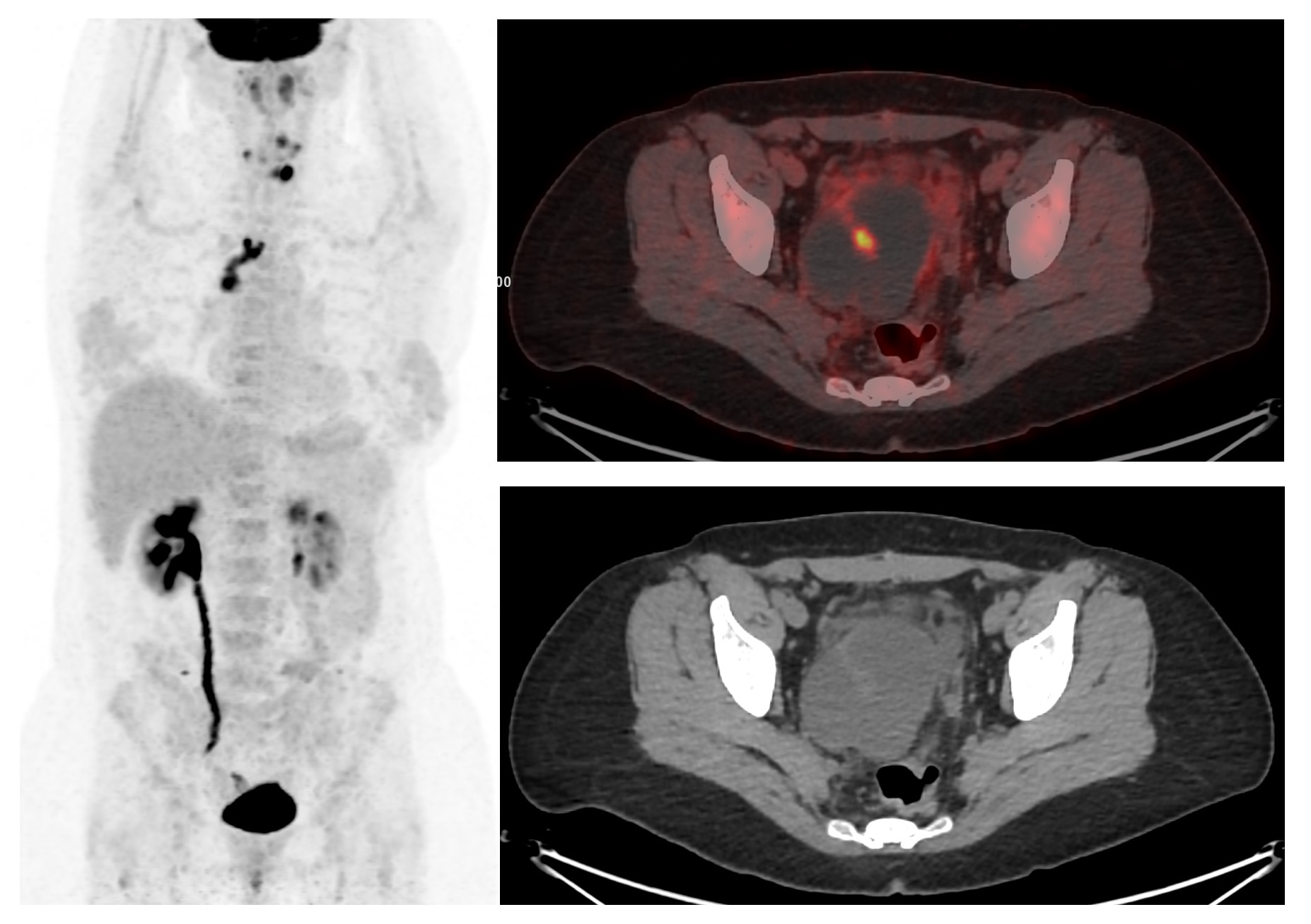
Figure 1: 18F-FDG PET/CT stimulated with Recombinant Thyroid-Stimulating Hormone (rTSH) showing tumor remains in the anterior cervical region and a pelvic mass dependent on the right adnexa, of a cystic nature, septated with FDG uptake, with an SUVmax of 15,3, which partially compresses the ipsilateral ureter.
It was decided to postpone the treatment with 131I due to the acute abdominal pain that the patient presented and the suspicion of synchronous malignant neoplasm in the ovary.
Two days later, an oophorectomy + right adnexectomy was performed with an anatomopathological result of endometrioid cystadenoma.
Subsequently, the patient was treated with 131I, without incident.
Discussion
Thyroid-Stimulating Hormone (TSH) is a glycoprotein that has structural similarities to other hormones such as Luteinizing Hormone (LH), Human Chorionic Gonadotropin (hCG), and Follicle-Stimulating Hormone (FSH); likewise, the Thyroid-Stimulating Hormone Receptor (TSH-R) is a glycoprotein that has a common subunit for the aforementioned hormones [1-4].
Expression of the TSH-R is increased in thyroid cancer, as well as in other malignancies, where the interaction of TSH with its receptor has the potential to stimulate the growth of such neoplasms. It also promotes the production of vascular endothelial growth factor, contributing to angiogenesis [2,3].
Some studies have shown the expression of TSH-R and thyroid hormone receptors in the endometrium and ovaries of healthy women, with higher expression in ectopic endometrium compared to eutopic endometrium, where TSH stimulates epithelial proliferation, therefore it is believed to be involved in the growth of endometriotic lesions, which has been confirmed in studies with mice. It has even been proposed that a high level of TSH in the blood (>2.5 μIU/ml) could be a non-invasive marker for the diagnosis of endometriosis [1,3-5].
Endometriosis is a common gynecologic condition that can be visualized on 18F-FDG PET/CT and is useful in differentiating malignant from benign processes. In endometriomas, FDG uptake is generally weak, and a SUVmax of 4.0 has been proposed as a cut-off point to differentiate from their malignant transformation, although they can sometimes simulate malignant lesions. In our case, FDG uptake exceeded this threshold, although the pathology ultimately revealed benignity. This could be related to associated inflammatory changes [6-10].
Experimental studies showed that TSH stimulates glucose transport and Glut1 expression in cultured thyroid cells. For this reason, it has been proposed to perform the 18F-FDG PET/CT study in differentiated thyroid cancer, previously stimulating with rTSH to increase FDG uptake by malignant cells, although mixed results have been obtained in this regard [11-13].
Conclusion
Due to all of the above, we propose that in this case the exogenous administration of rTSH may have precipitated the growth of the endometrioma, which was evidenced in our PET/CT study.
References
- Peyneau M, Kavian N, Chouzenoux S, Nicco C, Jeljeli M, Toullec L, et al. Role of thyroid dysimmunity and thyroid hormones in endometriosis. Proc Natl Acad Sci U S A. June 11, 2019; 116: 11894-9.
- Vieira IH, Rodrigues D, Paiva I. The mysterious universe of the TSH receptor. Front Endocrinol. July 2022; 13: 944715.
- Svensson A, Roth B, Kronvall L, Ohlsson B. TSH receptor antibodies (TRAb) – A potential new biomarker for endometriosis. Eur J Obstet Gynecol Reprod Biol. 2022; 278: 115-21.
- Sun SC, Hsu PJ, Wu FJ, Li SH, Lu CH, Luo CW. Thyrostimulin, but not thyroid-stimulating hormone (TSH), acts as a paracrine regulator to activate the TSH receptor in mammalian ovary. J Biol Chem. 2010; 285: 3758-65.
- Birke L, Baston-Büst DM, Kruessel JS, Fehm TN, Bielfeld AP. Can TSH level and premenstrual spotting constitute a non-invasive marker for the diagnosis of endometriosis? Birke et al. BMC Womens Health. 2021; 21: 336.
- Kusunoki S, Ota T, Kaneda H, Kimura M, Terao Y, Takeda S. Analysis of positron emission tomography/computed tomography in patients to differentiate between malignant transformation of endometrioma and endometrioma. Int J Clin Oncol. 2016; 21: 1136-41.
- Jeffry L, Kerrou K, Camatte S, Metzger U, Lelièvre L, Talbot JN, et al. Endometriosis with FDG uptake on PET. Eur J Obstet Gynecol Reprod Biol. 2004; 117: 236-9.
- Wang T, Xing Y, Zhao J. Endometriosis mimicking an advanced malignant tumor. Clin Nucl Med. 2016; 41: 648-9.
- Kitajima K, Ueno Y, Maeda T, Murakami K, Kaji Y, Kita M, et al. Spectrum of fl uorodeoxyglucose-positron emission tomography/computed tomography and magnetic resonance imaging fi ndings of ovarian tumors. Jpn J Radiol. 2011; 29: 605-8.
- Balogova S, Daraï E, Noskovicova L, Lukac L, Talbot JN, Montravers F. Interference of known or suspected endometriosis in reporting FDG PET/CT performed in another indication. Clin Nucl Med. 2022; 47: 305-13.
- Vera P, Kuhn-Lansoy C, Edet-Sanson A, Hapdey S, Modzelewski R, Hitzel A, et al. Does recombinant human thyrotropin-stimulated positron emission tomography with [18F]fluoro-2-deoxy-D-glucose improve detection of recurrence of well-differentiated thyroid carcinoma in patients with low serum thyroglobulin? Thyroid. 2010; 20: 15-23.
- Chin BB, Patel P, Cohade C, Ewertz M, Wahl R, Ladenson P. Recombinant human thyrotropin stimulation of fluoro-D-glucose positron emission tomography uptake in well-differentiated thyroid carcinoma. J Clin Endocrinol Metab. 2004; 89: 91-5.
- Saab G, Driedger AA, Pavlosky W, McDonald T, Wong CYO, Yoo J et al. Thyroid-stimulating hormone–stimulated fused positron emission tomography/computed tomography in the evaluation of recurrence in 131I-negative papillary thyroid carcinoma. Thyroid. 2006; 16: 267-72.