
Case Report
Austin J Obstet Gynecol. 2023; 10(3): 1221.
Spontaneous Heterotopic Pregnancy: As One of the Most Challenging Emergency Cases in Obstetrics
Fatima Katti¹*; Ebraheem Jawabrah¹; Huda Barghash¹; Mohammad Abbas Katti²; Haitham Abbassi³
¹Department of Obstetrics and Gynecology, Damascus University, Damascus, Syria
²Faculty of Medicine, Damascus University, Damascus, Syria
³Head of Department of Obstretrics and Gynecology, Damscus University, Damascus, Syria
*Corresponding author: Fatima Katti Department of Obstetrics and Gynecology, Damascus University, Damascus, Syria. Email: fatimakatti95@gmail.com
Received: August 03, 2023 Accepted: September 18, 2023 Published: September 25, 2023
Abstract
Spontaneous Heterotopic Pregnancy “SHP”: is defined as the presence of multiple gestations, in which, intrauterine and extrauterine pregnancy occur simultaneously, it is a life-threatening condition that requires immediate and accurate diagnosis and treatment.
Here, we present a case of a 38-year-old pregnant female who conceived spontaneously, at her sixth week of gestation, was presented to the emergency department with acute pain in lower abdomen and minimal vaginal bleeding, she underwent previous falsely reassuring ultrasound imaging for two times and her symptoms were ignored until the diagnosis was finally made by us. Pelvic ultrasound showed evidence of an IUP and a left adnexal mass, raising suspicion for a heterotopic pregnancy. An urgent exploratory laparotomy and a left salpingectomy were performed, postoperative, the patient recovered well but she had an early pregnancy loss at 8 weeks of gestation.
Clinicians should keep in mind that confirmation of an Intrauterine Pregnancy (IUP) should not preclude the existence of a heterotopic pregnancy.
Keywords: Spontaneous heterotopic pregnancy; Case report; Diagnosis; In vitro fertilization
Introduction
The coexistence of intrauterine pregnancy and ectopic pregnancy is called a Heterotopic (HT) pregnancy.
It is usually a consequence of Assisted Reproductive Technologies "ART" such as IVF and induction of ovulation, with an estimated incidence at between 1 to 3 in 100 pregnancies [1,2]. But there are cases that occur in the absence of any risk factor, in these cases, a spontaneous heterotopic pregnancy "SHP" represents a huge diagnostic challenge due to the rarity of the condition on the one hand (its incidence in the natural conceptions is: 1 per 30000 pregnancies) [1,2] and on the other hand it is a life-theratening condition that may be fatal to the mother if the diagnosis is delayed.
We brought the light to this rare case of SHP resulting from a normal conception without any risk factor, in which, the diagnostic opportunity was missed more than once which led to delay the diagnosis.
Case Presentation
A 38-year-old pregnant female (G3, P2) at her sixth week of gestation through natural conception with no previously fertility treatment, was presented to the emergency department with acute lower abdominal pain, most severe in the left side of the lower abdomen, associated with minimal vaginal bleeding, Obstetrical history included two spontaneous vaginal delivery. The medical, surgical, and family histories were unremarkable.
These symptoms started 5 days ago, and the patient consulted her doctor for this complaint, but he diagnosed an intrauterine pregnancy IUP, and attributed the interpretation of the symptoms as being due to fatigue caused by travel (the patient had returned from Germany a few days ago). However, the pain persisted and increased in intensity which prompted her to see another obstetrician, and again the symptoms were explained by being normal and may accompany any pregnancy! Unfortunately, the patient was sent home to return after two days later to our hospital with acute abdomen and hemodynamic instability: (her pressure was 80/50 mmHg, heart rate was 120 beats/min, there was also weakness and generalized paleness).
The clinical examination of the abdomen revealed guarding, rigidity and severe rebound tenderness of the lower abdomen which was pronounced in the left iliac fossa. The vaginal examination showed a closed cervix with motion tenderness as well as there was blood in the vaginal vault.
On further investigation, transvaginal ultrasonography was performed and showed intra uterine gestational sac measuring 5 weeks and 5 days (Figure 1). A left adnexal mass measured 5.3×6.4 cm, but no fetal pole was identified (Figure 2). The right adnexa were normal. There was also a medium volume of free fluid in the pelvis (Figure 3).
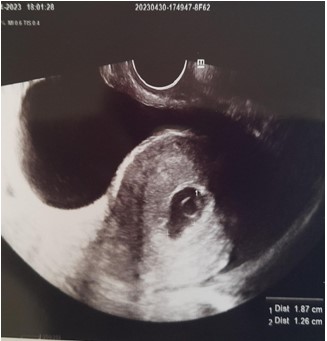
Figure 1: Transvaginal ultrasound demonstrates an intrauterine gestational sac measures 1.87*1.26 cm which correlates to the gestational age of 5 weeks and 5 days.
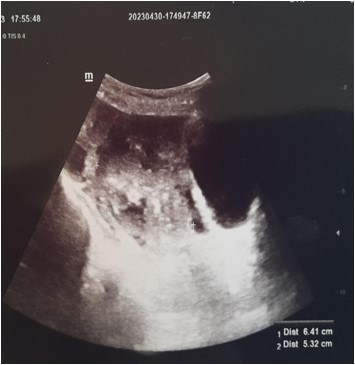
Figure 2: Transvaginal ultrasound showing a left adnexal mass measured 5.3×6.4 cm.

Figure 3: Transvaginal ultrasound demonstrates a medium volume of free fluid in the pelvis.
Laboratory data upon admission showed a white blood cell count of 7500 element/mm3, a hematocrite of 26.4% and serum hemoglobin concentration of 8, 8g/dl. Bhcg level of 14033, 51 IU/m. The patient was urgently prepared for the operating room by opening two large venous lines,and an initial resuscitation has begun with normal saline solutions.
Based on the clinical, laboratory, and imaging findings, the diagnosis of heterotopic pregnancy was established.
The patient was counseled on the risk of having an early pregnancy loss with the surgical intervention.
Due to the instability of the patient's hemodynamic status, an emergency exploratory laparotomy was performed under general anesthesia through pfannenstiel incision, leading to a finding of an enlarged left fallopian tube and a ruptured ectopic pregnancy with hemoperitoneum (Figure 4). Both the ovaries appeared normal. Approximately "1000 ml" of blood was evacuated from the peritoneal cavity by the suction. A total left salpingectomy was performed and a drain was placed in the abdominal cavity.

Figure 4: Intraoperative finding of ruptured left fallopian tube and hemoperitoneum.
Two units of blood and two fresh frozen plazma were transfused to the patient during and after the surgery. Histopathological result of the specimen confirmed chorionic villi suggestive of an ectopic pregnancy (Figure 5). Postoperative ultrasound confirmed a vital IUP and the patient was discharged from the hospital after one day. Follow up confirmed an early pregnancy loss at approximately 8 weeks of gestation.
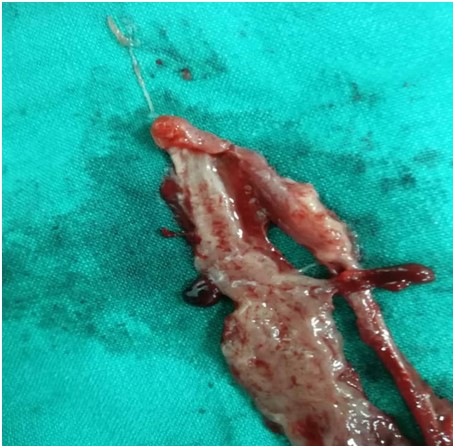
Figure 5: Surgical specimen, showing small fragment of the left ruptured uterine tube.
Discussion
The occurrence of spontaneous heterotopic pregnancies without risk factors is rare, but could be life-threatening if missed.
Our patient did not have any risk factor, the major risk factors for HP are same as those for ectopic pregnancy: (previous history of EP, tubal surgery, pelvic inflammatory disease "PID", smoking, use of an intrauterine device "IUD", and ART) [3].
The clinical symptoms of HP are unspecific, this means it can be found in several other gynecological and nongynecological medical conditions which makes the differential diagnosis very wide.
The patient had a reassuring initial ultrasound demonstrating a live IUP: there is a prior sonoghraphy of normal IUP in at least a third of the cases [4].
The TVUS showed (IUP, adnexal mass and free fluid) raising suspision for a HP: the TVUS is the gold standard for diagnosis a HP, However its sensitivity has been found to range from 26,3% to 92.4%, [5], therefore, we must always link between the results of ultrasound images and the clinical findings.
The intervention was done through an emergency laparotomy due to the instabiity of the case, while if the diagnosis had been made early, a conservative therapeutic approach could have been chosen, laparotomy causes uterine irritability which increases the rate of IUP loss, according to several studies, the total abortion rate was 26.56% in all HP patients and the abortion rate in surgical management was 25.93% [6,7] so the standared treatment for HP is the conservative surgery preferably by laparoscopy, for that reason we should always be strive to make the diagnosis as early as possible.
Conclusion
The delayed diagnosis of this condition leads to serious consequences including: ruptured of the ectopic pregnancy, hypovolemic shock, maternal mortality and postoperative intrauterine pregnancy loss, therefore, our most important goal through this case is to increase the clinical suspicion index in order to avoid misdiagnosis.
Considering the importance of heterotopic pregnancy, clinicians should pay special attention to carefully check the adnexa, even after confirming presence of an intra uterine pregnancy, to rule out heterotopic pregnancy.
Author Statements
Funding Information
The authors received no funding regarding the publication of this article.
Conflict of Interest
The authors declare that there is no conflict of interest to be reported.
Consent
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
References
- Ouafidi B, Kiram H, Benaguida H, Lamrissi A, Fichtali K, Bouhya S. Diagnosis and management of a spontaneous heterotopic pregnancy: rare case report. Int J Surg Case Rep. 2021; 84: 106184.
- Kajdy A, Muzyka-Placzynska K, Filipecka-Tyczka D, Modzelewski J, Stanczyk M, Rabijewski M. A unique case of diagnosis of a heterotopic pregnancy at 26 weeks - case report and literature review. BMC Pregnancy Childbirth. 2021; 21: 61.
- Aziz M, Arronte J. A case of spontaneous heterotopic pregnancy in natural conception complicated with hemoperitoneum. Heliyon. 2020; 6: e03373.
- Nguyen KP, Hudspeth M, Milestone H. Spontaneous heterotopic pregnancy: diagnosis and management. Case Rep Obstet Gynecol. 2022; 2022: 2994808.
- Ouafidi B, Kiram H, Benaguida H, Lamrissi A, Fichtali K, Bouhya S. Diagnosis and management of a spontaneous heterotopic pregnancy: rare case report. Int J Surg Case Rep. 2021; 84: 106184.
- Li JB, Kong LZ, Yang JB, Niu G, Fan L, Huang JZ, et al. Management of heterotopic pregnancy: experience from 1 tertiary medical center. Med (Baltim). 2016; 95: e2570.
- Cerniauskaite M, Vaigauskaite B, Ramašauskaite D, Šilkunas M. Spontaneous heterotopic pregnancy: case report and literature review. Medicina (Kaunas). 2020; 56: 365.