
Case Report
Austin J Obstet Gynecol. 2022; 9(3): 1208.
Actinomycosis Simulating Malignancy on CT: A Case of A Long-Forgotten IUD
Jose E1, Ch ng YZ2, Oyekan OA3, Chauhan CM4 and Alabi A5
1General Surgery SHO, Frimley Park Hospital, Surrey, United Kingdom
2Obstetrics & Gynaecology, Frimley Park Hospital, Surrey, United Kingdom
3General Surgery SHO, Frimley Park Hospital, Surrey, United Kingdom
4General Surgery SHO, Frimley Park Hospital, Surrey, United Kingdom
5General Surgery Consultant, Frimley Park Hospital, Surrey, United Kingdom
*Corresponding author: Elenza Jose Department of General Surgery, Frimley Health Foundation Trust, Frimley Park Hospital, Portsmouth Rd, Frimley, Camberley GU16 7UJ, UK
Received: November 11, 2022; Accepted: December 16, 2022; Published: December 22, 2022
Abstract
Actinomycosis simulating malignancy on CT: A case of a longforgotten IUD
Actinomyces Israelii is known to be commensal, particularly in the gums and tonsils, sometimes in the vagina. The diagnosis of actinomycosis is challenging owing to nonspecific clinical findings. First instance imaging often resembles inflammatory and infective pathologies like Crohn’s or intestinal tuberculosis, and in this case, abdominal malignancies [1]. Actinomycosis infectionsare complicated by their tendency to extend into surrounding structures and develop fistulae [2]. Our case report specifically looks at a fit-and-well female patient who had been referred under a suspected gastrointestinal cancer pathway after a recent change in bowel habit for CT imaging which was subsequently thought to be disseminative malignant growths. Our 56-year-old lady had an indurating mass in her abdomen draining pus which prompted her GP to discuss this case with the surgeons. On further MRI imaging and lab cultures, it was revealed that the sinister mass is found to be an Actinomyces Israelii colonised long-forgotten IUD placed 12 years ago. The unfortunate patient suffered widespread abdominal involvement which required extensive surgery involving major bowel resection, salpingo-oopherectomy, bilateral ureteric stents for hydronephrosis and a partial cystectomy.
Keywords: Actinomycosis, Salpingitis, Oophoritis, Abscess, Laparotomy, Cystectomy, IUD, Fistula
Case report
A 56-year-old female presented at her GPs complaining ofa change in bowel habit for the past 10 weeks and felt a lump in her abdomen associated with some unintentional weight loss. Otherwise fit and well, she was referred on a suspected lower gastrointestinal cancer pathway for CT imaging of both chest and pneumo-colon. This was reported as disseminated abdominal- pelvic malignancy from a possible right adnexal primary. It was found there was a direct extension of the disease into the subcutaneous fat of the anterior abdominal wall which became concerning when the central mass in her abdomen began ulcerating and discharging pus, for which her GP referred to the surgical assessment unit.
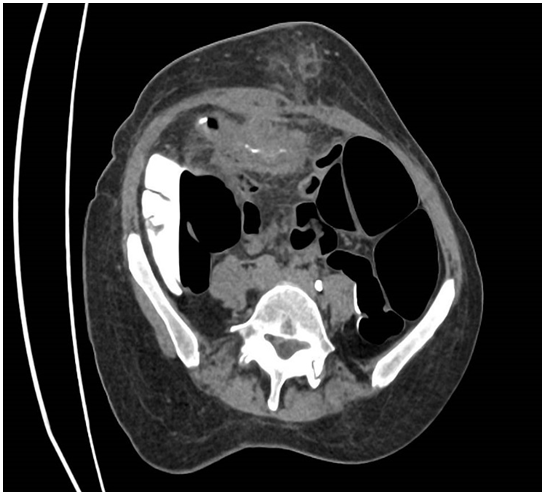
Figure 1: Axial view of a CT Pneumocolon showing luminal narrowing
in the sigmoid with extensive infiltrative peritoneal and
omental disease and concomitant disease extension into the anterior
abdominal wall and subcutaneous.

Figure 2: Coronal view of Ct pneumocolon with additional right
adnexal part solid part cystic mass displacing the uterus to the patient’s
left and Incidental Simple.

Figure 3: Sagittal View of CT showing the IUD in situ and a clearer
view of the infiltrating mass.
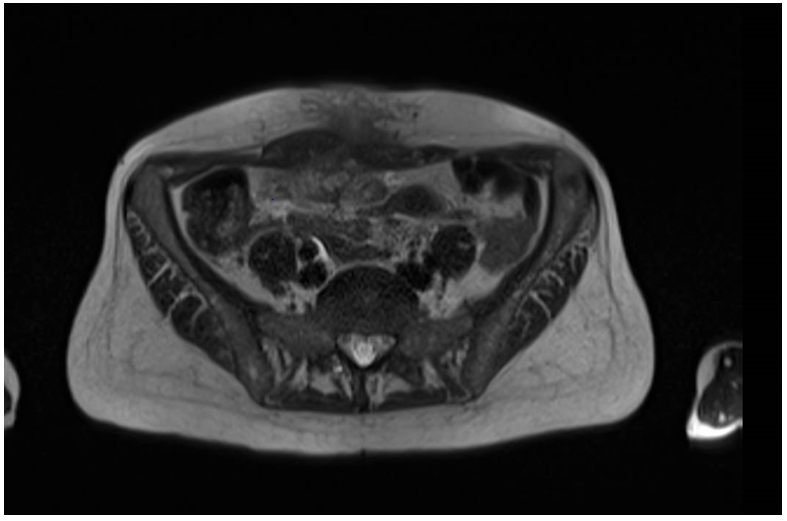
Figure 4: MRI showing suspected bilateral adnexal abscesses
and more superiorly spreading this enteric inflammation which fistulates
through the anterior abdominal wall.
On examination, her abdomen was soft but showed hard mass over the suprapubic region, extending up to below the umbilicus (measuring about 10 x 10cm) with small indurating ulcers seen on the surface.
Her case was discussed at the colorectal multi-disciplinary meeting and had a plan for an ultrasound-guided percutaneous biopsy the same day. It was found the dermis of the anterior abdominal wall had mild oedema within the subcutaneous fat, however, no discrete mass or collection could be found. Her inflammatory markers at that time showed WCC16.9, Hb 96, CRP 86 also proved to be concerning but not overtly so.
An MRI of pelvis was requested, and it was thought to bilateral adnexal abscesses and more superior spreading of the enteric inflammation involving fistulas draining through the anterior abdominal wall. Unfortunately, there was also a new right-sided hydronephrosis from the extrinsic compression of ureters by the pelvic mass. This pelvic „mass“ is now thought to be secondary to a retained IUD. As these extensive findings are unlikely to resolve with conservative management, the patient was listed for an emergency complex laparotomy with extra involvement of both the gynaecology and the urology team.
This patient underwent laparotomy approach with small bowel resection, right hemicolectomy plus anterior resection with formation of loop ileostomy. It was discovered the bladder had an involvement thus needed repair for which she had a partial cystectomy. The gynaecology team took over for a right salpingo-oopherectomy, left salpingectomy and of course, removal of the IUD. Urology was also present as she required temporary bilateral ureteric stents for hydronephrosis. The pelvic abscesses were drained, and Robinson drains left to pelvis.
Her pus culture came back positive for Actinomyces Israelii. The histopathologic examination of the bowel, bladder, ovaries and fallopian tubes showed fibrino-purulent inflammatory process as well as actinomyces organisms with active chronic fistulating abscess. She was started on daily doses of IV Ceftriaxone for 6 weeks in total. Following that, microbiology advised for oral Amoxicillin tablets to be started for 6months after the IV course had finished. The patient has recovered well from the surgery and was discharged home with daily visits to our outpatient parenteral antibiotic service for the duration of her course of IV Ceftriaxone.
The patient was also followed up with a cystogram suggesting no evidence of urinary extravasation, but bilateral reflux noted to the renal pelvises. She has been recovering well since the operation with no complications.
Discussion
Pelvic actinomycosis is ultimately a rare finding. Timely diagnosis and interventions can reduce long-term complications and avoid life-changing events. Management strategy, once a retained IUD is established, should include immediate commencement on long-term antibiotics and removal surgery to avoid complications and further reoccurrence [3]. The role of imaging including MRI of abdomen was vital as it showed fistulae through the anterior abdominal wall, with the involvement of bowel. Although the clinical picture was ambiguous, actinomycosis should be thought about in differential diagnoses when suspicion of malignancy appears on the CT, particularly septic patients with long-term intrauterine devices in-situ.
References
- Yegüez JF, Martinez SA, Sands LR, Hellinger MD. Pelvic actinomycosis presenting as malignant large bowel obstruction: a case report and a review of the literature. Am Surg. 2000; 66: 85–90.
- Garner JP, Macdonald M, Kumar PK: Abdominal actinomycosis. Int J Surg. 2007; 5: 441–448.
- Valour F, Senechal A, Dupieux C, Karsenty J, Lustig S, et al. Actinomycosis: Etiology, clinical features, diagnosis, treatment, and management. Infect Drug Resist. 2014; 7: 183–97.