
Case Series
Austin J Otolaryngol. 2024; 10(1): 1133.
Could the NOSE Score Predict the Success of Septoplasty?
Rihab Lahmar¹; Mohamed Masmoudi¹; Mohamed Dhaha²; Azer Chebil¹; Mehdi Hasnaoui¹; Khalifa Mighri¹
¹Department of Head and neck Surgery, Tahar Sfar Hospital Mahdia, Tunisia
²Department of Head and neck Surgery, Salah Azaez oncology Institute Tunis, Tunisia
*Corresponding author: Rihab Lahmar Head and neck surgery department, University of Monastir, Tahar Sfar Hospital Mahdia, Tunisia. Tel: +216 92 816 474 Email: rihab.lahmar.med@gmail.com
Received: March 18, 2024 Accepted: April 17, 2024 Published: April 24, 2024
Abstract
Objective: To assess outcomes of septoplasty using a validated subjective questionnaire: Nasal Obstruction & Symptom Evaluation (NOSE) score.
Materials and methods: Two hundred fifty patients undergoing septoplasty were included in our study. The NOSE score was documented preoperatively and postoperatively. Results were analyzed and compared statistically. Results: In our study, severe (NOSE scale >50) and moderate nasal obstruction (NOSE scale between 26 and 50) were correlated with success of septoplasty and there were considered as predictive factors of successful surgery (p<0.001). Mild nasal obstruction (NOSE scale between 0 and 25) was correlated with septoplasty failure but this finding was not statistically verified (p = 0.09).
Conclusion: Subjective scales like NOSE questionnaire can be used to perform pre- and postoperative assessment in patients undergoing septoplasty.
Keywords: Nasal obstruction; NOSE score; Septoplasty; Nasal septum deviation
Introduction
Nasal obstruction is a common complaint in otolaryngology associated with a decreased quality of life [1].
Nasal septum deviation is the leading cause of such obstruction and can only be corrected surgically [2,3].
Septoplasty is the surgical procedure recommended to treat these patients. There are many subjective and objective methods for assessing outcomes after nasal surgery. However, there is no agreement on the nasal obstruction assessment tool. Postoperative physical examination and nasal endoscopy have been used in previous studies to evaluate the effectiveness of septoplasty, but it depends on the examiners perspective [1,2,4].
Many questionnaires were developed to assess symptoms, a specific clinical problem, quality of life, and effectiveness of a treatment of chronic diseases. The Nose score is a series of questionnaires used in the fiel of rhinology, which is introduced by Stewart et al. This score is specific for nasal obstruction and it is easy to complete for patient [1,5].
In our study, we have chosen this questionnaire because the NOSE score can be applied for the outcome after septoplasty and can be used as a predictor of successful surgery [1].
The Aims of the Study
Using the NOSE score to evaluate functional symptoms, particularly nasal obstruction before and after surgery, in patients undergoing septoplasty to improve outcomes.
Materials and Methods
We conducted a retrospective study in the ENT department of Taher Sfar Mahdia; Tunisia, over a 7-year period (January 2013 to December 2018) that included 250 patients who underwent septoplasty.
Inclusion Criteria:
1. Patients aged 18 to 65 years
2. Symptomatic deviated nasal septum that causes chronic nasal obstruction
3. Postoperative follow -up for at least 12 months
Exclusion Criteria:
1. Patients with previous nasal septal surgery
2. History of chronic rhino sinusitis, nasal polyposis, allergic rhinitis, inferior turbinate hypertrophy, inflammatory diseases, and craniofacial malformations.
A general physical examination and an ENT examination were performed: includes an anterior rhinoscopy and preoperative nasal endoscopy.
After informed written consent, patients were asked to complete questionnaires describing the severity of their symptoms using the Nasal Obstruction Symptom Evaluation Scale: NOSE scale (Figure 1).
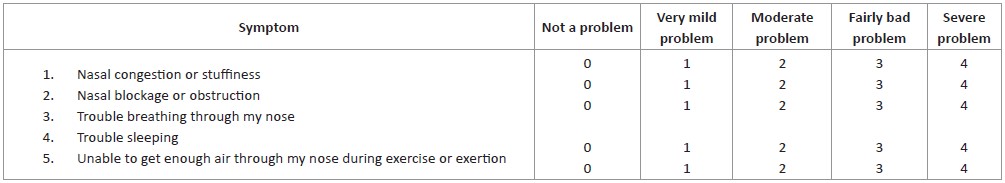
Figure 1: The Nasal Obstruction Symptom Evaluation Scale: NOSE scale.
It included five questions related to nasal congestion, nasal blockage or obstruction, difficulty breathing, sleep problems, and difficulty during physical exercise.
The score for each question varied between 0 and 4. Each score was multiplied by 5 to generate an overall score between 0 and 100.
Nasal obstruction was classified into the following categories:
- Moderate: between 26 and 50
- Mild: between 0 and 25
Statistical Methods
Statistical analyzes were performed with SPSS version 22.0 (SPSS Inc., Chicago II).
Statistical tests used:
- Pearson's Chi2 test for qualitative variables if the number of subgroups is >5.
- Fisher's exact test for qualitative variables if the subgroup size is <5.
Statistical significance was defined as p<0.05.
Results
A total of 250 patients were included in our study.
The patients were predominantly men with a sex ratio of 1.4 (145 men and 105 women).
The patients ranged in age from 18 to 62 years (mean 32.7 years).
The NOSE score allowed them to be divided into 3 groups (Figure 2):
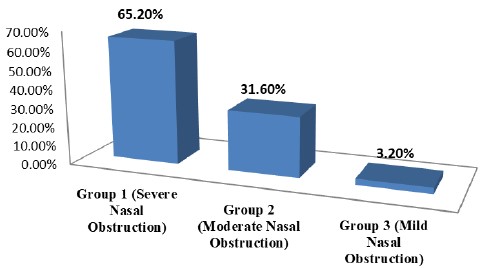
Figure 2: Preoperative distribution of NOSE scores (N=250).
- Group 1: patients with severe nasal obstruction: 65.2% of cases (163 patients) with a mean preoperative NOSE score of 70/100
- Group 2: patients with moderate nasal obstruction: 31.6% of cases (79 patients) with a mean preoperative NOSE score of 42/100.
- Group 3: patients with mild nasal obstruction: 3.2% of cases (8 patients) with a mean preoperative NOSE score of 24/100.
Postoperatively, all patients in group 1 had an improvement in the NOSE score
The average NOSE score went from 70/100 to 18.3/100 at 3 months, an improvement of 51.7 points (Figure 3).
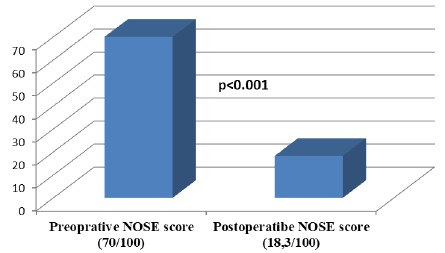
Figure 3: Comparison of pre and postoperative NOSE score in Group1 (N=163).
This improvement was considered significant (p-value <0.001).
Therefore, severe nasal obstruction (NOSE scale>50) was considered a predictive factor
of successful surgery.
For group 2, the mean NOSE score went from 42/100 before the operation to 19.3/100 after the operation (Figure 4).
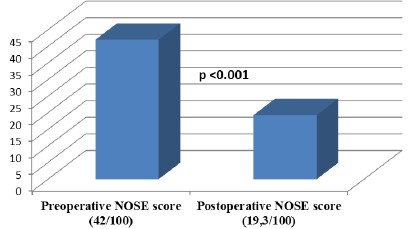
Figure 4: Comparison of pre and postoperative NOSE score in Group 2 (N=79).
This score was reduced by 22.7 points: this improvement is considered significant (p<0.001).
Moderate nasal obstruction (NOSE scale between 26 and 50) was correlated with the success of septoplasty surgery.
For group 3, the NOSE score went from 24/100 preoperatively to 30/100 postoperatively (Figure 5).
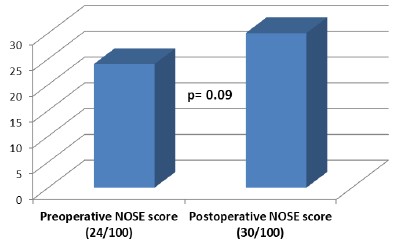
Figure 5: Comparison of pre and postoperative NOSE score in Group 3 (N=8).
In fact, five patients kept the same NOSE score: they showed no improvement.
The rest of this group (three patients) reported a worsening of their nasal obstruction with a NOSE score lower than the preoperative score.
Mild nasal obstruction (NOSE scale between 0 and 25) was correlated with septoplasty failure, but this finding was not statistically verified (p = 0.09).
Discussion
The effects of septoplasty on quality of life have not been widely studied in the literature.
The success rate of septum surgery varies between 63% and 85% [6,7].
The results perceived by patients vary considerably depending on the different degrees of satisfaction, ranging from complete disappearance of symptoms to total failure [1].
Postoperative and postoperative evaluation of symptoms is important: it makes it possible to compare different surgical techniques, share experiences between surgeons, and to self-evaluate [1,8].
In the literature, two types of means of functional evaluation of results (after septoplasty) have been described: subjective and objective means [7,9].
The study by André et al. did not find any arguments to favor one method over another [10].
Rhinomanometry and Acoustic Rhinometry allow an objective assessment of nasal obstruction [1,11].
According to Gordon, 22% of septoplasty patients still report complaints of nasal obstruction after surgery, despite improvements in their rhinomanometry results [12].
Another study by Kahveci et.al. found that the clinical use of Rhinometry is limited: it can only show changes in volume and area changes inside the nose [1,13].
In our study, no objective functional exploration was carried out due to the lack of means.
The NOSE scale is a nasal-specific questionnaire that can be used to assess nasal obstruction in a group of patients. It can be used to evaluate the outcome of different surgical therapies. It can be used to compare the effect of medical versus surgical therapy [5,14]. It is a reliable, valid, and sensitive tool. It has been validated for use for preoperative and postoperative evaluation.
It appears to be the most appropriate tool for the subjective assessment of nasal obstruction [14,15].
The study by Stewart et al has also used the NOSE score for subjective evaluation as was used in our study, and the data revealed a significant improvement in the mean NOSE score ((67.5 versus 23.1, p < 0.0001), at 3 months after septoplasty ,which remained stable after 6 months [1,2,14].
In our study, the patient satisfaction rate was also significantly high with the NOSE score for groups 1 and 2.
Many studies have shown that patients with significant initial functional symptoms benefit better from surgery than patients with moderate or fluctuating symptoms: this improvement was also detectable after 6 months.
The study by Shukla et al. compared the efficacy of the NOSE score & the Visual Analog Scale (VAS) in determining the symptomatic benefit in patients undergoing septoplasty: The NOSE score showed a higher improvement and a better patient satisfaction rate when used to measure nasal obstruction as compared to the VAS score [2].
There are other complexes, valid and nose-specific questionnaires, which have the advantage of assessing different rhinological parameters in addition to nasal obstruction: we can cite
Chronic sinusitis survey-, Rhino sinusitis outcome measure, Sino-Nasal outcome test, and RhinoQOL. We note that these tools were originally designed to assess chronic rhino sinusitis [2,13].
Conclusions
Septoplasty is the standard treatment for Deviated Nasal Septum (DNS).
However, the perception of the benefits of septoplasty varies considerably between patients, ranging from complete improvement of symptoms to total failure.
Using the NOSE score will help to let the patient know the expected outcome as a result.
Severe and moderate preoperative nasal obstructions were considered predictive factors.
of successful surgery.
Postoperative evaluation makes it possible to compare different surgical techniques, share and compare experiences between surgeons, and self-evaluate.
Finally, evaluating the results makes it possible to improve them.
References
- Dutta A, Goyal L. Can Nose Scale Be Used as a Predictor of Successful Surgery in Patients Undergoing Septoplasty. Indian Journal of Otolaryngology and Head & Neck Surgery. 2020; 74: 1-7.
- Shukla RH, Nemade SV, Shinde KJ. Comparison of visual analogue scale (VAS) and the Nasal Obstruction Symptom Evaluation (NOSE) score in evaluation of post septoplasty patients. World journal of otorhinolaryngology-head and neck surgery. 2020; 6: 53-8.
- Moore M, Eccles R. Objective evidence for the efficacy of surgical management of the deviated septum as a treatment for chronic nasal obstruction: a systematic review. Clinical otolaryngology: official journal of ENT-UK; official journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery. 2011; 36: 106-13.
- Hardcastle P, White A, Prescott R. Clinical or rhinometric assessment of the nasal airway—which is better? Clinical Otolaryngology & Allied Sciences. 1988; 13: 381-5.
- Stewart MG, Witsell DL, Smith TL, Weaver EM, Yueh B, Hannley MT. Development and validation of the Nasal Obstruction Symptom Evaluation (NOSE) scale. Otolaryngology—Head and Neck Surgery. 2004; 130: 157-63.
- Andrades P, Cuevas P, Danilla S, Bernales J, Longton C, Borel C, et al. The accuracy of different methods for diagnosing septal deviation in patients undergoing septorhinoplasty: a prospective study. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2016; 69: 848-55.
- Mondina M, Marro M, Maurice S, Stoll D, de Gabory L. Assessment of nasal septoplasty using NOSE and RhinoQoL questionnaires. European Archives of Oto-Rhino-Laryngology. 2012; 269: 2189-95.
- Griffin JE, Caloss R. Nasal deformities. Atlas of the oral and maxillofacial surgery clinics of North America. 2004; 12: 31-74.
- Lee SB, Jang YJ. Treatment outcomes of extracorporeal septoplasty compared with in situ septal correction in rhinoplasty. JAMA Facial Plastic Surgery. 2014; 16: 328-34.
- Binnetoglu A. A Combined Approach to Crooked Nose Deformity. Aesthetic Plast Surg. 2016; 40: 360-6.
- Tomkinson A, Eccles R. Acoustic rhinometry. Current Opinion in Otolaryngology & Head and Neck Surgery. 1996; 4: 7-11.
- Bezerra TFP, Stewart MG, Fornazieri MA, Pilan RRdM, Pinna FdR, Padua FGdM, et al. Quality of life assessment septoplasty in patients with nasal obstruction. Brazilian journal of otorhinolaryngology. 2012; 78: 57-62.
- Kahveci OK, Miman MC, Yucel A, Yucedag F, Okur E, Altuntas A. The efficiency of Nose Obstruction Symptom Evaluation (NOSE) scale on patients with nasal septal deviation. Auris Nasus Larynx. 2012; 39: 275-9.
- Sundh C, Sunnergren O. Long-term symptom relief after septoplasty. European Archives of Oto-Rhino-Laryngology. 2015; 272: 2871-5.
- Bonaparte JP, Campbell R. A prospective cohort study assessing the clinical utility of the Cottle maneuver in nasal septal surgery. Journal of Otolaryngology-Head & Neck Surgery. 2018; 47: 45.