
Review Article
Austin J Public Health Epidemiol. 2024; 11(2): 1163.
Review on Climate Change and One Health
Tewodros Legesse*
Addis Ababa University College of Veterinary Medicine and Agriculture Department of microbiology, Immunology and Veterinary Public Health MSC Flower, Ethiopia
*Corresponding author: Tewodros Legesse Addis Ababa University College of Veterinary Medicine and Agriculture Department of microbiology, Immunology and Veterinary Public Health MSC Flower, Ethiopia. Email: tewoderos.legesse@aau.edu.et
Received: May 16, 2024 Accepted: June 06, 2024 Published: June 13, 2024
Summary
Climate change is a result of the global increase in average air and ocean temperatures, and rising average sea levels. Livestock production and health are significantly vulnerable to the impact of climate change. The objective of this review is demonstrate advantages of integrated One Health approaches compared to conventional separated public and animal health approaches. Climate change has direct and indirect impacts on emerging and re-emerging animal diseases and zoonoses since it disrupts natural ecosystems and allows disease-causing pathogens to move into new areas where they may harm wild life and domestic species, as well as humans. Climate change affects diseases and pest distributions, range prevalence, incidence and seasonality but the degree of change remains highly uncertain. The occurrence and distribution of vector borne diseases such as bluetongue, west nile fever, rift valley fever, African horse sickness, etc. are closely associated with weather patterns and long-term climatic factors strongly influence the incidence of outbreaks. The interaction between animal production and climate change is complex and multidirectional since animal production contributes to climate change; but to the reverse and worse condition, climate change highly affects animal production. Climate change, animal production systems and animal diseases are strongly linked each other. But what is worse is that both change in climate and the production systems of animals highly affect the occurrence, distribution, emergence and reemergence of animal diseases. Therefore, addressing climate change is critical to protecting and promoting the health of all species on the planet. The one health approach is particularly useful in addressing climate change as it provides a frame work for recognizing the complex relationships between human, animal and environmental health and for developing solutions that benefit all three.
Keywords: African horse sickness; Bluetongue; Climate; Climate change; West Nile Fever; Rift Valley Fever; One health
Abbreviations: WNV: West Nile Virus; WHO: World Health Organization; LRTI: Lower Respiratory Tract Infections; URTI: Upper Respiratory Tract Infection; RSU: Respiratory Syncytial Virus; RV: Rhinovirus; SARS-Cov2: Sever Acute Respiratory Syndrome Coronavirus 2019.
Introduction
Economic activities increase the emission of greenhouse gases. This human-induced climate change is one of the global environmental changes. Raised Carbon Dioxide (CO2), methane, and other greenhouse gases. Increase the heat-trapping capacity of the lower atmosphere resulting in global warming [32]. There are informative documentations that suggest that among those that are believed to be particularly susceptible to climate change, developing nations take the most impact because of the dependence of livelihoods on climate sensitive sectors such as agriculture, tourism and fishery [16]. Above all these burdens, climate change has resulted in a significant drop in productivity on global considerations and this is a matter that predicts a huge threat to the stability of the whole food system and at its cost comes food insecurity [54]. Much earlier documents have notified that the effects of climate change are believed to have an interfering existence in the health and wellbeing of animals through heat related diseases and stress, extreme weather events, and emergence or re-emergence of infectious diseases, especially vector borne diseases [17].
Climate change is superposed by demographic, social and economic, environmental and landscape changes (Hwang et al., 2017) which often cannot clearly be separately delineated (de Anda 2017). Modifications in vector, reservoir and pathogen lifecycles as well as diseases of domestic and wild animals and plants are influenced by multiple complex processes [48]. This also applies to the disruption of synchrony between interacting species, trophic cascades and alteration or destruction of habitats (Patz and Hahn 2013; Stevenson et al., 2015). Previous studies and reviews have documented the multiple health impacts of climate change, including an increase in infectious diseases, respiratory disorders, heat-related morbidity and mortality, under nutrition due to food insecurity, and adverse health outcomes ensuing from increased sociopolitical tension and conflicts [53].
It has been clearly depicted that there is an urgent necessity to investigate the direct and indirect correlation of climate change with natural, biological and other human induced hazards as it will facilitate a more effective and helpful understanding and identification of cascading and complex hazards and risk in awell patterned manner to address climate change [57]. Under univocal and global agreement, the world has gathered on multiple protocols, signed numerous legislative agreements and assembled different patterns of mitigation strategies that integrate conventional mitigation strategies, new sets of innovation and technologies and principles of altering the earth’s radiation balance through the management of solar and terrestrial radiation [50].
Despite the existence of these strategies, with inefficient performances, there are reports that illustrate arise in temperature is to be expected between 2030 2052 and this was evident enough for an immediate development to favorable mitigation and adaptation mechanism [32]. With consideration to the complexity and uncertainties of climate change and its effects, an integrative and interdisciplinary approach namely “One Health” is found to be of a great significance to facilitate clearer understanding of climate change impacts on environment, animal and human health (Patz, 2012). There are setbacks observed for the practicality and effectiveness of this concept inconsequence of the impeded engagement of the medical community unlike the veterinarians who had given a much greater interest [29]. With considerations to the potential benefits from this collaborative tool, there needs to be a clearer understanding on the importance of promoting policies that integrate health and environmental concerns and its cruciality in mitigating the impacts of climate change and ensuring a sustainable future for all [49].
The objective of this review is to
i. Demonstrate advantages of integrated One Health approaches compared to conventional separated public and animal health approaches and Examine the potential of One Health to adaptation to effects of climate change.
Climate Change and Health
Climate change is affecting more than just physical infrastructure and economics as it is increasingly affecting basic natural life-support systems. It affects the fundamental requirements for health - safe drinking water, clean air, sufficient food, and secure shelter and has many adverse health impacts [32]. The impact on health results directly from extreme weather events (e.g. heat waves and floods) and indirectly from socially mediated risks (e.g. displacement, conflict, damaged infrastructure, crop failure) and/or ecologically mediated risks (e.g. food, water, vectors) [34].
The World Health Organization (WHO) developed standardized comparative risk assessment methods for estimating aggregate disease burdens attributable to different risk factors which have been applied to existing and new models for a range of climate-sensitive diseases in order to estimate the effect of global climate change on current disease burdens and likely proportional changes in the future [6].
They estimated that the extent of climate change by the year 2000 (relative to the 1961-1990 average climate) was estimated to have caused, worldwide during that year, approximately 160 000 deaths and the loss of 5 500 000 disability-adjusted life-years from malaria, malnutrition, diarrheal disease, heat waves and floods [6].
To comprehensively consider the impact of climate change, we have drawn from existing models developed by McMichael (2003) and Eisenberg (2007) and present an adapted model which is discussed in the following section. In assessing the health impact of climate change, one must, however, be mindful that the effects of climate change are complex, and often interact with other distal determinants of health (Eisenberg, 2007) and global environmental changes (McMichael, 2010).
Unequivocally, there is a warming of planet Earth since the 1950s, with increased temperatures of the atmosphere and the oceans. The amount of ice and snow has diminished; sea levels have risen; and an increased frequency of extreme weather. Events, heat waves, drought, floods, storms are observed in parallel to an increase of the concentration of greenhouse gases [32]. Climate change affects a large number of sectors. This means that integrated approaches and intersectional collaboration are essential to face such challenges.
The added value of one health to climate change adaptation may significantly contribute to the following contexts and issues: food security with particular emphasis on animal source foods, extensive livestock systems, especially the role of ruminant livestock, antimicrobial resistance control, environmental sanitation, and steps towards regional and global integrated syndromic surveillance and response systems. Arctic regions appeared as highly vulnerable to zoonotic disease [13,46], although other geographic regions like dry lands and mountains are also hotspots of climate change.
Diseases that are Occurred by Climate Change
According to the World Health Organization (WHO), the “climate change and global warming” are the greatest challenges of humanity in the twenty-first century. They threaten all aspects of our life. The WHO listed the health hazards on human health due to climatic changes into the following item (Figure 2): (1) direct and indirect effects of global warming, (2) stratospheric ozone depletion, (3) disturbance in terrestrial and marine ecosystems, (4) loss of biodiversity, (5) changes in the hydrological systems and freshwater supply, (6) Land degradation and loss of river deltas and coastal cities, (7) urbanization, deforestation and population dislocation/immigration, and finally (8) limited food production [55].
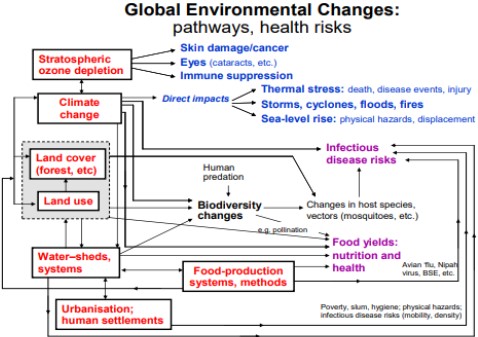
Figure 1: Global environmental changes: pathways and health risks
Figure 2: Effect of climatic changes on emerging of infectious diseases.
Figure 3: Frequency of responses by 306 Haramaya University health sciences students about different health effects of climate change, 2011.
Vector Borne Disease
Malaria: While the increase in temperature enables the survival of mosquitoes and the elongation of their season of activity, heavy rainfalls are also necessary to provide standing water surface required for egg-laying and larval development. High levels of air humidity enhance the vector population dynamics. Finally, the wind plays an important role in the spread of mosquitoes and their associated diseases. The wind was incriminated to be the reason for the emergence of Culex tritaeniorhynchus mosquitoes in several areas in China [51].
When we investigate the mosquito-borne diseases such as dengue fever, yellow fever, and chikungunya virus (transmitted by Aedes species), West Nile fever, Eastern equine encephalitis and heartworm infection (by several mosquito species including Anopheles, Aedes, Culex, Culiseta, Coquillettidia, Deinocerites, Mansonia, Orthopodomyia, Psorophora and Uranotaenia), Ross River fever and Usutu virus infection Culex and Aedes) and malaria (by Anopheles and Aedes) [44], we would notice that one mosquito species (Aedes aegypti) out of 3500 mosquito species is responsible for most serious outbreaks and can transmit most of the mosquito-borne pathogens outside Africa [43].
The emergence and expansion of A. albopictus in the Western Hemisphere enhanced the emergence and endemicity of A. albopictus-borne diseases like chikungunya virus infection and dengue fever in Italy, France and Croatia in Europe, and in Hawaii, Texas and Florida in USA. West Nile virus became now also endemic in North America after its emergence due to migratory birds [44].
Dengue Fever: Transmission of dengue viruses is influenced by climate, among many other factors (Gubler DJ 1988) [41]. Infectious agents that require cold-blooded invertebrate species in order to complete their life cycle are particularly sensitive to subtle changes in temperature. Dengue transmission is largely confined to tropical and subtropical regions because freezing temperatures kill over wintering larvae and eggs of Ae.aegypti mosquitoes [8]. Also, temperature strongly affects pathogen replication, maturation, and period of infectivity, as laboratory data suggest that the extrinsic incubation period (or viral development rate) shortens non linearly with higher temperatures, increasing the proportion of mosquitoes that become infectious at a given time [52]. Also, elevated temperatures can shorten insect survival time or disrupt pathogen development.
West Nile virus: West Nile Virus (WNV) is insect borne virus which induces fatal encephalitis in mammals, humans and even birds. The virus is transmitted by Culex mosquitoes. Like other mosquito-borne diseases, the disease expanded its geographic range to emerge in new countries as a result of climatic changes. The disease emerged in South America in 2003 and induced a large outbreak in Europe in 2010 (involved Greece, Romania, Hungary, Spain, Russia, Turkey and Italy) [42]. The disease was also detected in other European countries such as France, Portugal and Serbia. The source of the invading viruses was confirmed to be from Israel, Morocco and Turkey. Later on, in 2018, the virus emerged for the first time in Germany [59]. In 1999, WNV first emerged in New York (USA), the increase in mosquito population due to the increase rainfalls and the lengthening of the mosquito activity season due to the increase in temperature leads to the increase of the prevalence of the disease. In 2013, 2170 cases of WNF were reported in USA with 88 fatalities [42].
Lyme Disease: Environmental change is considered as the main driver of the shifts in the distribution of vectors and hosts, and hence of disease emergence [21]. Climate and the local habitat change could interact and affect the dispersal and movement of the species involved in the transmission cycle of Lyme disease in a complex manner. For example, a warmer climate with milder winters and earlier spring snowmelt may shift the phenology of the white-footed mouse breeding activity and dispersal, with higher activity and movement earlier in the season. Increased activity in turn alters the rate of encounter between this host and its pathogens, affecting the dynamics of transmission cycle of B. burgdorferi [37]. On the other hand, fragmentation of host habitat may reduce host population size, limit host dispersal, and alter host densities and diversity [12] (Li et al., 2012).
Respiratory Illnesses
Climate change, air pollution, and viral respiratory infection are highly interconnected, and without interventions to halt global warming, we can expect the burden of viral respiratory disease to increase worldwide. More than 90% of the world's population is exposed to polluted air. Convincing epidemiologic data has linked air pollution exposure with increased incidence of viral respiratory infections like Upper Respiratory Tract (URI) infections. bronchitis, and Lower Respiratory Tract Infections (LTRI) such as pneumonia and bronchiolitis. Similarly, temperature, humidity, and extreme weather events have also been directly and indirectly associated with respiratory infections (Jin X et al., 2019).
Viral respiratory tract infections are most common illnesses in humans, with estimated 17 billion incident cases globally in 2019. Common viruses causing respiratory tract infection include influenza, Respiratory Syncytial Virus (RSV), Rhinovirus (RV), and SARS-CoV-2. Viral respiratory infection imposes a substantial burden on populations and health systems. Non- influenza viral respiratory infections were estimated to cost the US economy $40 billion annually. Viruses are also the primary trigger for acute asthma exacerbations and a major cause of COPD exacerbations. While most viral respiratory infections are mild and self-limited, they can lead to severe complications in susceptible patients, including pneumonia and even respiratory failure. The SARS-CoV-2 pandemic in particular has contributed to over 3 million deaths worldwide [28].
Food Born and Water Born Disease
Water-borne and food borne diseases are a serious public health concern worldwide. Water-borne and food borne outbreaks are closely associated with climatic changes and disturbances in the ecosystem. They are more common in the summertime and increase with rising temperatures and humidity [23]. In addition, among the expected climate changes is the increase in frequencies of floods and heavy rainfalls due to warming of the oceans and due to the increase in frequency and strength of Al Nino and Hurricanes. This, in turn, will be reflected on the increase in water-borne diseases as giardiasis, cryptosporidiosis, and infections with pathogenic E. coli, Shigella, cholera, Salmonella, and viral hepatitis A [24].
The most famous water-borne disease is the cholera, a bacterial diarrheal disease caused by Vibrio cholerae. The disease is transmitted by drinking contaminated water. Cholera is a highly temperature-dependent disease which increases with the increase in water temperature. Infection due to Vibrio spp. is an example of the influence of global warming and ecology on the emergence of pathogens [48].
Climatic factors can also promote the spread of non-infectious diseases (e.g. the increase in humidity, temperature and rainfalls enhance the growth of fungi and the spread of mycotoxin related diseases). In warm summer, many factors interact leading to the increase in cases of food poisoning such as enhanced bacterial survival, the people spend more time outside where they eat and drink, and finally due to the increase in the insect/rodent population and activity [39].
Impact of Climate Change in Ethiopia Related to Diseases
Climate change is of critical importance to Ethiopia. Mainly due to changes in the climate, Ethiopia has faced recurrent droughts across its different parts. This has been more observable particularly since the 1970s. The population size of Ethiopia and the impact of the activities of the growing population have increased dramatically over the last decades [11]. There are frequent changes in the climate. These changes are often followed by droughts. Not only Ethiopia but many other African countries have also often fallen victim to these changes. Facing challenges associated with climate change has since recently become global trends. The mean annual temperature has, for example, increased by 1.3°C between the years 1960 and 2006. This is estimated to be an average rate of 0.28°C increase in temperature per decade [15].
Ethiopia is one of the countries vulnerable to climate change and losses of human lives from flooding, domestic water supply shortages, malnutrition and the altitudinal extension of malaria transmission are increasingly being reported. Flooding is one of the climates related hazard that affects human health in several ways such as death, injuries, water-borne diseases, malnutrition, and mental ill health [31]. In addition, millions of dollars’ worth of property were damaged in Dire Dawa, and about 10,000 livestock of the Afar ethnic groups perished in the floods [3].
Climate change-induced malaria has also been reported in the Afar region [3], and in South Omo. In both places the rate of flooding has increased and a large area has come under permanent flooding. This has triggered the infestation of bush and mosquitoes (malaria) [19]. Climate change is feared to expose an additional 2 billion people worldwide to dengue transmission by the 2080s [25]. Dengue transmission is projected to significantly widen in the area where the snail-borne disease schistosomiasis occurs. On the other hand, Visceral Leishmaniasis (VL) has become a growing health problem in Ethiopia. The annual burden of VL is estimated to be between 4,500 and 5,000 cases [58].
Ethiopia was identified as a "hotspot" for zoonotic disease events. The country ranked number one hotspot for leptospirosis, the fourth largest hotspot for Q fever and Trypanosomosis, and the tenth for tuberculosis. Much of the burden of zoonosis (68%) is distributed among only 13 countries. Ethiopia has the 4th highest burden caused by zoonosis [22]. These data indicate an already existing burden of zoonotic disease in the country. The burden has the potential to be exacerbated by the effects of climate change. Researchers have identified an association between outbreaks of leptospirosis and extreme rainfall and flooding in a wide range of countries with different ecologies.
Cases of reported water-borne diseases, such as unspecific dysentery and diarrheal cases, increased in Ethiopia from 19,980 in 2008 to 116,571 in 2011 [34]. Malnutrition is one of the climate related impacts that affects mainly the growth of children, and the distribution of malnutrition among children in Ethiopia has been associated with the occurrence of drought. Based on climate change projections, annual mean temperatures are projected to increase over the coming decades in Ethiopia (UNDP, 2008). These changes could contribute to malnutrition among under- five children. Increasing temperatures are also facilitating the spread of vector- borne diseases, particularly malaria, from lower altitudes to the Ethiopian highlands as a result of increasing temperatures [3].
Conclusion and Recommendation
The world’s climate is changing at a faster rate. Even though changes in climate and extreme weather events have received increased attention in the recent years; climate change is real and is happening now with concomitant changes in precipitation, flooding, winds and frequency of extreme events. The average temperature in the world has increased in the last few years compared to the previous century and is expected to continue rising. Climate change can have direct and indirect effects on infectious diseases through disrupting natural ecosystems and providing more suitable environments for infectious diseases allowing disease-causing bacteria, viruses, and fungi to move into new areas where they may harm wild life and domestic species, as well as humans and it is exacerbating diseases in livestock. The distribution and incidence of vector borne diseases are directly influenced by climate since the geographical distributions of vectors are pre-determined by temperature and humidity. Animal production and climate change are inter-linked in complex and multidirectional ways; i.e. animal production systems can be sources of climate change through releasing gases and deforestation for production of animal feed; while, climate change affects animal production through desertification, water scarcity, changes in feed (availability, access, and appropriateness) etc. But, both the change in climate and production systems of animals have impacts on diseases of animals; as a result, leading to low productivity of animals, the impact being devastating in developing countries. This suggests that climate change, animal production and animal diseases are closely related and influence each other through different mechanisms. So, working integrated with other fields are the most important thing to control impacts of climate change, for this the one health approach are the most important.
Based on the current review, the following recommendations are forwarded:
Awareness creation, in working in an integrated systematic manner, should be made to the stakeholders in the environmental conservation, animal production and animal health.
Sustainable animal farming and land use, and climate adaptation and mitigation strategies should be developed.
Researches with emphasis given to the state of climate change and the direct and indirect effects it poses on animal production and on the occurrence and distribution of animal diseases should be conducted.
Improving one health approach are useful for collaborative work with other related fields.
Establishing climate change and health research centers equipped with adequate laboratory facilities, and developing and strengthening national and international research collaborations are other essential areas.
Author Statements
Acknowledgment
First and foremost, I would like to give my praise to God, for his love and mercy on me and to St. virgin Marry for help in every aspect of my life. My grateful gratitude goes to my respect full advisor Dr. Olana Merera for his interesting support, intellectual guidance, and devotion of their very precious time to correct this paper.
References
- Ababa A. A Climate Change Country Assessment Report for Ethiopia. 2011.
- Baker MG, Kvalsvig A, Zhang J, Lake R, Sears A, Wilson N. Declining Guillain-Barre syndrome after campylobacteriosis control, New Zealand, 1988–2010. Emerging infectious diseases. 2012; 18: 226.
- Biru A, Adem A, Eshete B, Hailu B, Mahmud M, Temesgen D. Afar National Regional State Programme of plan on adaptation to climate change. Semera: Environmental Protection Authority of the Federal Democratic Republic of Ethiopia. 2010.
- Bless PJ, Schmutz C, Suter K, Jost M, Hattendorf J, Mäusezahl-Feuz M, et al. A tradition and an epidemic: determinants of the campylobacteriosis winter peak in Switzerland. European journal of epidemiology. 2014; 29: 527-537.
- Bohr J. Reporting on climate change: A computational analysis of US newspapers and sources of bias, 1997–2017. Global Environmental Change. 2020; 61: 102038.
- Campbell S, Remenyi TA, White CJ, Johnston FH. Heatwave and health impact research: A global review. Health & place. 2018; 53: 210-218.
- Cerutti R, Pirinen E, Lamperti C, Marchet S, Sauve AA, Li W, et al. NAD+-dependent activation of Sirt1 corrects the phenotype in a mouse model of mitochondrial disease. Cell metabolism. 2014; 19: 1042-1049.
- Chandler AC. Factors influencing the uneven distribution of Aedes aegypti in Texas cities. American Journal of Tropical Medicine. 1945; 25: 145-149.
- Chandler AC. Factors influencing the uneven distribution of Aedes aegypti in Texas cities. American Journal of Tropical Medicine. 1945; 25.
- Chua PL, Dorotan MM, Sigua JA, Estanislao RD, Hashizume M, Salazar MA. Scoping review of climate change and health research in the Philippines: a complementary tool in research Agenda-Setting. International journal of environmental research and public health. 2019; 16: 2624.
- Conway D, Schipper ELF. Adaptation to climate change in Africa: Challenges and opportunities identified from Ethiopia. Global environmental change. 2011; 21: 227-237.
- Daszak P, Cunningham AA, Hyatt AD. Anthropogenic environmental change and the emergence of infectious diseases in wildlife. Acta tropica. 2001; 78: 103-116.
- Dudley JP, Hoberg EP, Jenkins EJ, Parkinson AJ. Climate change in the North American Arctic: a one health perspective. EcoHealth. 2015; 12: 713-725.
- Enserink M. Questions abound in Q-fever explosion in the Netherlands. 2010.
- Ethiopian EPA. Ethiopia’s climate-resilient green Economy (CRGE). Federal Democratic Republic of Ethiopia, Addis Ababa, Ethiopia. 2011; 188.
- Ford JD, Berrang-Ford L, Bunce A, McKay C, Irwin M, Pearce T. The status of climate change adaptation in Africa and Asia. Regional Environmental Change. 2015; 15: 801-814.
- Forman S, Hungerford N, Yamakawa M, Yanase T, Tsai HJ, Joo YS, et al. Climate change impacts and risks for animal health in Asia. Rev Sci Tech Off Int Epiz. 2008; 27: 581-597.
- Galaz V, Leach M, Scoones I, Stein C. The political economy of One Health research and policy. 2015.
- GebreMichael Y, Kifle M. Local innovation in climate-change adaptation by Ethiopian pastoralists. Addis Ababa, Ethiopia. 2009.
- Gellynck X, Messens W, Halet D, Grijspeerdt K, Hartnett E, Viaene J. Economics of reducing Campylobacter at different levels within the Belgian poultry meat chain. Journal of food protection. 2008; 71: 479-485.
- Gould EA, Higgs S. Impact of climate change and other factors on emerging arbovirus diseases. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2009; 103: 109-121.
- Grace D, Mutua F, Ochungo P, Kruska RL, Jones K, Brierley L, et al. Mapping of poverty and likely zoonoses hotspots. 2012.
- Greer A, Ng V, Fisman D. Climate change and infectious diseases in North America: the road ahead. Cmaj. 2008; 178: 715-722.
- Haines A, Patz JA. Health effects of climate change. Jama. 2004; 291: 99-103.
- Hales S, De Wet N, Maindonald J, Woodward A. Potential effect of population and climate changes on global distribution of dengue fever: an empirical model. The Lancet. 2002; 360: 830-834.
- Jin X, Ren J, Li R, Gao Y, Zhang H, Li J, et al. Global burden of upper respiratory infections in 204 countries and territories, from 1990 to 2019. E Clinical Medicine. 2021; 37: 100986.
- Kojwang HO, Larwanou M. An overview of nationally appropriate mitigation actions (NAMAs) and national adaptation programmes of action (NAPAs) in Africa. International Forestry Review. 2015; 17: 103-113.
- Lavine JS, Bjornstad ON, Antia R. Immunological characteristics govern the transition of COVID-19 to endemicity. Science. 2021; 371: 741-745.
- Mackenzie JS, Jeggo M. The One Health approach—Why is it so important?. Tropical medicine and infectious disease. 2019; 4: 88.
- Mahoo HF, Radeny MA, Kinyangi J, Cramer L. Climate change vulnerability and risk assessment of agriculture and food security in Ethiopia: which way forward?. CCAFS Working Paper. 2013.
- Manuta J, Lebel L. Climate change and the risks of flood disasters in Asia: crafting adaptive and just institutions. In International Workshop on Human Security and Climate Change, University of Chiang Mai, Chiang Mai, Thailand. 2005.
- Masson-Delmotte V, Zhai P, Pörtner HO, Roberts D, Skea J, Shukla PR. Global Warming of 1.5°C: IPCC Special Report on Impacts of Global Warming of 1.5°C above Pre-industrial Levels in Context of Strengthening Response to Climate Change, Sustainable Development, and Efforts to Eradicate Poverty. Cambridge University Press. 2022.
- Mäusezahl D, Karanja S, Crump L, Hartinger S, Nooh F, Schelling E, et al. Climate change and One Health. FEMS Microbiol Lett. 2018; 65: fny085.
- MOH E. Federal Democratic Republic of Ethiopia Ministry of health health sector development program IV October 2010 contents. 2014.
- Monath TP. Dengue. The Arboviruses; Ecology and Epidemiology. 1988; 2: 224-260.
- Ogden NH, Lindsay LR. Effects of climate and climate change on vectors and vector-borne diseases: ticks are different. Trends in parasitology. 2016; 32: 646-656.
- Ogden NH, Bigras-Poulin M, Hanincova K, Maarouf A, O’callaghan CJ, Kurtenbach K. Projected effects of climate change on tick phenology and fitness of pathogens transmitted by the North American tick Ixodes scapularis. Journal of Theoretical Biology. 2008; 254: 621-632.
- Pachauri RK, Allen MR, Barros VR, Broome J, Cramer W, Christ R, et al. Climate change 2014: synthesis report. Contribution of Working Groups I, II and III to the fifth assessment report of the Intergovernmental Panel on Climate Change. 2014; 151.
- Park MS, Park KH, Bahk GJ. Interrelationships between multiple climatic factors and incidence of foodborne diseases. International journal of environmental research and public health. 2018; 15: 2482.
- Paternoster G, Babo Martins S, Mattivi A, Cagarelli R, Angelini P, Bellini R, et al. Economics of One Health: Costs and benefits of integrated West Nile virus surveillance in Emilia-Romagna. PloS one. 2017; 12: e0188156.
- Patz JA, Epstein PR, Burke TA, Balbus JM. Global climate change and emerging infectious diseases. Jama. 1996; 275: 217-223.
- Paz S. Climate change impacts on West Nile virus transmission in a global context. Philosophical Transactions of the Royal Society B: Biological Sciences. 2015; 370: 20130561.
- Powell JR. Mosquito-borne human viral diseases: why Aedes aegypti?. The American journal of tropical medicine and hygiene. 2018; 98: 1563-1565.
- Redshaw CH, Stahl-Timmins WM, Fleming LE, Davidson I, Depledge MH. Potential changes in disease patterns and pharmaceutical use in response to climate change. Journal of Toxicology and Environmental Health, Part B. 2013; 16: 285-320.
- Roth F, Zinsstag J, Orkhon D, Chimed-Ochir G, Hutton G, Cosivi O, et al. Human health benefits from livestock vaccination for brucellosis: case study. Bulletin of the World health Organization. 2023; 81: 867-876.
- Ruscio BA, Brubaker M, Glasser J, Hueston W, Hennessy TW. One Health–a strategy for resilience in a changing arctic. International Journal of Circumpolar Health. 2015; 74: 27913.
- Schmutz C, Mäusezahl D, Bless PJ, Hatz C, Schwenkglenks M, Urbinello D. Estimating healthcare costs of acute gastroenteritis and human campylobacteriosis in Switzerland. Epidemiology & Infection. 2017; 145: 627-641.
- Semenza JC, Herbst S, Rechenburg A, Suk JE, Höser C, Schreiber C, et al. Climate change impact assessment of food-and waterborne diseases. Critical reviews in environmental science and technology. 2012; 42: 857-890.
- Viegas S. Climate Change and the need of a One Health Approach–from science to policy. European Journal of Public Health. 2021; 31: ckab164-271.
- Fawzy S, Osman AI, Doran J, Rooney DW. Strategies for mitigation of climate change: a review. Environmental Chemistry Letters. 2020; 18: 2069-2094.
- Walsh AS, Glass GE, Lesser CR, Curriero FC. Predicting seasonal abundance of mosquitoes based on off-season meteorological conditions. Environmental and Ecological Statistics. 2008; 15: 279-291.
- Watts DM, Burke DS, Harrison BA, Whitmire RE, Nisalak A. Effect of temperature on the vector efficiency of Aedes aegypti for dengue 2 virus. ARMY MEDICAL RESEARCH INST OF INFECTIOUS DISEASES FORT DETRICK MD. 1987; 36: 143-52.
- Watts N, Amann M, Arnell N, Ayeb-Karlsson S, Beagley J, Belesova K, et al. The 2020 report of the Lancet Countdown on health and climate change: responding to converging crises. The lancet. 2021; 397: 129-170.
- Wheeler T, Von Braun J. Climate change impacts on global food security. Science. 2013; 341: 508-513.
- WHO. (WHO report 2017: Global environmental change). 2017.
- Wilkes M, Papageorgiou S, Kim TY, Baldrias L, Aguilar E, Kelly T, et al. One Health workers: innovations in early detection of human, animal, and plant disease outbreaks. Journal of Global Health Reports. 2019; 3: e2019093.
- Zhang R, Tang X, Liu J, Visbeck M, Guo H, Murray V, et al. From concept to action: a united, holistic and One Health approach to respond to the climate change crisis. Infectious Diseases of Poverty. 2022; 11: 1-6.
- Zhou XN, Yang GJ, Yang K, Wang XH, Hong QB, Sun LP, et al. Potential impact of climate change on schistosomiasis transmission in China. The American journal of tropical medicine and hygiene. 2008; 78: 188-194.
- Ziegler U, Lühken R, Keller M, Cadar D, Van Der Grinten E, Michel F, et al. West Nile virus epizootic in Germany, 2018. Antiviral research. 2019; 162: 39-43.