
Special Article: Coronary Artery Bypass Surgery
Austin J Surg. 2023; 10(3): 1309.
Standard CABG – Pain Killers or Extending Life?
Bhavsar R¹; Tang M²; Nielsen PH²; Jakobsen CJ²*
1Department of Anesthesiology, South Jutland hospital, Denmark
2Heart, lung and vessel, Aarhus University Hospital, Denmark
*Corresponding author: Jakobsen CJ Heart, lung and vessel, Aarhus University Hospital, 8200 Aarhus N, Denmark. Tel: +45 40105200 Email: cjj@dadlnet.dk
Received: August 18, 2023 Accepted: September 11, 2023 Published: September 18, 2023
Abstract
During the last decades, several studies have shown improved short- and long-time survival after Coronary Artery Bypass Grafting (CABG). Despite the greater reduction in postoperative mortality, there is still a concern whether cardiac surgery is primarily palliative pain relieving and delaying mortality or offers survival equal to or better than the background population.
Method and Results: The study was based on 19,948 single CABG patients performed from 2000-2020, obtained from the mandatory Western Denmark Heart Registry and not previous exposed to cardiac surgery.
Overall, the mortality declined from the first to the last 5-year study period, with 63.6% in 1-year mortality and 41.1% in 5-year mortality. Gender perspective evaluation revealed significant differences. The female mortality was, except for the last 5-year period, significantly higher than men (5.21% vs 3.73% in 1-year mortality, P<0.0001), underlined further by men almost balancing the population mortality after 5 years, while females never caught up. Comorbidity and postoperative complications had great negative impact on survival, but even without comorbidity or complications, females constantly showed higher mortality than the female population. Thus, the definitive result showed a remarkable difference between genders, comparing the study group and population 10-year survival, being 69.3% vs 63.8% in men and 64.3% vs 68.8% in females.
Conclusions: Females have a substantial higher mortality than males after CABG when compared to the background population. Males seem to catch up with population mortality 4-5 years after surgery, while females continue to have a lower survival than the background population.
Keywords: CABG; Complications; Comorbidity; Mortality
Abbreviations: ACS: Acute Coronary Syndrome; BIMA: Bilateral Internal Mammary Arteries; CABG: Coronary Arterial Bypass Grafting; CAG: Coronary Angiography; CPB: Cardiopulmonary Bypass; CPR: Central Personal Register; CL: Confidence Limit; ECC: Extra Corporeal Circulation; IHD: Ischaemic Heart Disease; IQR: Interquartile Range; ICU: Intensive Care Unit; INR: International Normalized Ratio; LMW: Low Molecular Weight; LIMA: Left Internal Mammary Artery; OR: Odds-Ratio; PCI: Percutaneous Coronary Intervention; RBC: Red Blood Cells; RIMA: Right Internal Mammary Artery; WDHR: Western Denmark Heart Registry
Introduction
Ischaemic Heart Disease (IHD) has been the main cause of death in both genders worldwide for more than three decades [1-2]. Significant differences have been described between the genders in prevalence, treatment, and outcome of IHD [3-5]. Previously, IHD was considered a similar entity in men and women with just a decade delay with the risk of underestimating the importance of sex-specific differences, like the reported difference of the impact of diabetes and smoking [6-7].
The number of Danes with cardiovascular diseases has in creased by 20% since 2006. The most frequent is IHD with approximately 1/3 of the patients, of which again, 1/3 have had a myocardial infarction [8]. Despite the higher incidence, the number of patients dying from cardiac diseases has been halved during the last 25 years, presumably due to increased prevention and better treatments, especially after myocardial infarction [9]. Before 2010, mortality was equal in men and women, but since then the decline has been greatest in females [8].
Previous studies concluded that females were hit by cardiovascular disease 7-10 years later than males [10-11]. This delay could not fully explain the disharmony between equal number of deaths and the big difference in registered cardiovascular procedures. The conclusion was that in females, both acute and chronic presentation of IHD, was underdiagnosed and less treated than among males [10] and additionally females more often suffered from postprocedural complications like heart failure, pulmonary oedema, and death [11]. This is underlined in cardiac surgery where the EuroSCORE estimates a higher perioperative mortality in females compared to men with equal age and comorbidity [12-13].
Several studies have shown long time survival after Coronary Artery Bypass Grafting (CABG) [14-15], but despite the greater reduction in postoperative mortality after standard cardiac procedures, there is still some concern, whether cardiac surgery is primarily palliative or extend the study group living time [16-17]
The aim of this study was to evaluate mortality after standard CABG, primarily with focus on expected survival from the background population together with impact of age, gender, and comorbidity factors to categorize and map factors relevant in the treatment cardiovascular diseases.
Materials and Methods
Data Source
This study was based on adult patients undergoing single CABG, registered in the Western Denmark Heart Registry (WDHR).WDHR registration, mandatory for all adult cardiovascular procedures, was established in 1999 with three public and one semi-public (since 2005) cardiac surgery centre and fully functional by the end of 2000. The clinical registry covers approximately 60% of the Danish uptake area, and holds detailed patient-, risk-, procedure-, and care-related data, together with in-hospital postoperative complications.
Data are collected and registered prospectively and is an integral part of clinical practice [18]. Data quality is controlled by automatic validation rules at data entry combined with systematic validation procedures, random spot checks and regular updates. Major updates have been carried out twice, mainly increasing the number of obligatory data fields, and since 2006 all data related to this study have been obligatory. Data registered before 2006 is, according to handling and procedures at the time, considered as 0 or negative, if any other data was registered on the specific formulas.
All Danish citizens have a unique Civil Personal Registration number (CPR number) assigned at birth and kept throughout the entire life, enabling cross-linking between different Danish health and civil registries, giving access to relevant follow up on all procedures and medical treatments.
Patients submitted to standard CABG were considered eligible for the study. Patients without valid CPR number, previous cardiac surgery were, together with a small number with incomplete data registration, excluded from the analysis revealing a cohort of 19,948 patients (Figure 1). The study was registered by the Danish Data Protection Agency (1-16-02-455-21). The agency's rules for the use and handling of data were met and written consent is not required for registry-based studies according to Danish legislation.
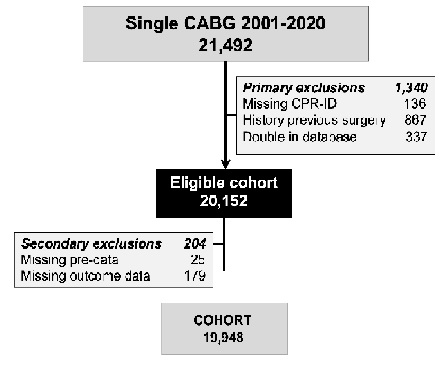
Figure 1: Single CABG and Aortic valve replacement procedures and CABG + aortic valve replacement 2001-2020. Exclusions are in-valid ID, previous cardiac surgery and missing relevant info.
Factors and Outcome
The primary outcome was all cause mortality after specified periods. The analysis was primarily based on age, gender, coronary anatomy, comorbidity, and perioperative complications. The registered complications were acute myocardial infarction, stroke, new dialysis, re-exploration due to bleeding, prolonged time in ICU (=72 hours or return after discharge) and ventricular fibrillation/tachycardia, together with treatment factors like perioperative inotropes and massive blood transfusion (=7 units) indicating a complicated postoperative path. Coronary Angiography (CAG) before and after the surgery was obtained from the WDHR and grouped as preoperative examination (0-90 days before surgery) and postoperative 30-days and 1-year as a potential complicated path.
Background Population Mortality
Due to great differences in average living age for men and women, and especially the relatively large change in population average living time over the study period, all patients were assigned the supposed risk of death, founded on the official 5-year life tables from Statistics Denmark (Figure 2) [19]. Thus, all patients were allocated an individual 1- and 5-year mortality, based on the time of surgery, age and gender. Following, study group actual mortality can be analyzed against background population mortality in a 1:1 ratio in subgroups of gender, and selected factors in question. The approach seems a valid approach, especially due to great changes in living time in the primary surgical timespan from 60 to 80 years of age.
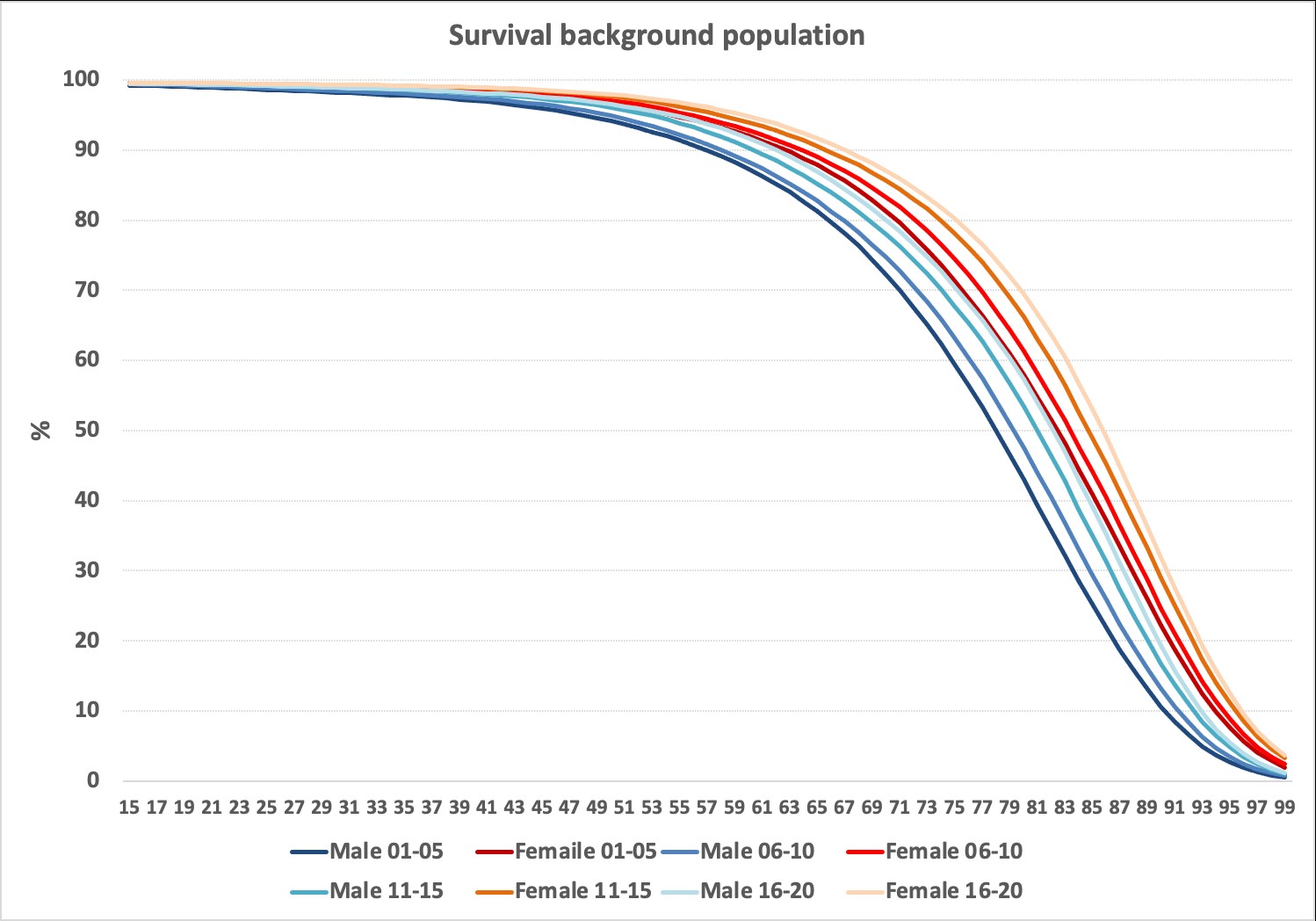
Figure 2: Population background survival divided on 5-year periods and gender. Survival curves based on one year mortality of the actual ages (15-99 years; Data from Danish Statistics). https://www.dst.dk/en/
Statistical Analyses
The detailed statistical analysis was primarily based on patients divided on gender, comorbidity and postoperative complications. To avoid too small groups, data was gathered in time groups where appropriate. Categorical variables were primarily analysed using the Χ2-test, while in longitudinal data was used students-independent t-test or Mann-Whitney independent test depending on data-normality in group or parameter analysis, while ANOVA or Kruskal-Wallis was used for comparisons between subgroups. When evaluating outcomes over time statistical analysis was based on Kaplan-Meier survival curves and compared to results of individual assigned population mortality. Analyses were performed with MedCalc® software version 20.008 (Mariakerke, Belgium). A probability value of <0.05 was used to define statistical significance.
Results
The WDHR contained 21,492 eligible procedures from 2001-2020. A few foreigners or refugees without a valid CPR number (136) preventing follow-up after discharge and accordingly not eligible for survival follow-up were excluded, together with 1,204 with previous cardiac surgery and 204 with incomplete registered data, leaving a cohort of 19,948 CABG procedures (Figure 1).
The patient characteristics show relatively great differences over time in most registered parameters (Table 1). Although statistically significant, the difference in median age was low, went up and down and was likely without clinical importance. The fraction of females declined gradually from 20.1% to 15.5% in last 5-year period. The number of patients without comorbidity increased and the number with high and moderate comorbidity declined over time. Patients with diabetes as well as patients not discontinuing their antiplatelet drugs increased. Thus, according to EuroSCORE, factors with both positive and negative impact on the outcome changed over the observation time. The risk score seemed higher in females, mainly due to the age and gender, as the “raw” comorbidity in the study group was only marginal higher in females.
Factor
2001-2005
2006-2010
2011-2015
2016-2020
p-value
Male
Female
p-value
Number patients
6,493
4,686
5,110
3,659
16,242
3,706
Female (fraction)
1302(20.1)
923(19.7)
914(17.9)
567(15.5)
<0.0001#
Age (years)
65.6±9.7
66.3±10.3
66.4±10.0
66.3±9.5
<0.001
65.7±9.2
68.0±9.3
<0.001
No-comorbidity
1044(16.1)
1650(35.2)
2107(41.2)
1634(44.7)
<0.0001#
5276(32.5)
1159(31.3)
<0.0001#
Low comorbidity (1-2)
2669(41.1)
1358(29.0)
1604(31.4)
1225(33.5)
5671(34.9)
1185(32.0)
Moderate comorbidity (3-5)
2246(34.6)
1244(26.5)
1154(22.6)
694(19.0)
4283(26.4)
1055(28.5)
High comorbidity (> 5)
465(7.2)
428(9.1)
245(4.8)
106(2.9)
958(5.5)
286(7.7)
Risk score
4.87±3.14
5.05±3.47
4.68±3.21
4.41±2.96
<0.001
4.45±3.14
6.23±3.04
<0.001
Age and gender score
2.13±1.71
2.24±1.82
2.25±1.77
2.18±1.62
<0.001
1.93±1.58
3.37±1.64
<0.001
Comorbidity score
2.68±2.29
2.66±2.60
2.21±2.24
1.89±2.02
<0.001
2.35±2.31
2.68±2.38
<0.001
Surgery type/non-elective
0.09±0.94
0.15±1.03
0.21±1.07
0.34±1.11
<0.001
0.18±1.02
0.19±1.05
0.149
No diabetes
5071(78.1)
3647(77.8)
3891(76.1)
2721(74.4)
<0.0001#
12596(77.6)
2734(73.8)
<0.0001#
New/diet treatment
210(3.2)
127(2.7)
128(2.5)
73(2.0)
441(2.5)
97(2.6)
Tablet treatment
380(5.9)
356(7.6)
433(8.5)
324(8.9)
1109(6.8)
384(10.4)
Insulin dependent
447(6.9)
490(10.5)
641(12.5)
457(12.5)
1667(10.3)
368(9.9)
Off-pump surgery
1154(17.8)
1163(24.8)
1065(20.8)
602(16.5)
<0.0001#
3181(19.6)
803(21.7)
0.0002#
Non-elective
289(4.5)
345(7.4)
545(10.7)
615(16.8)
<0.0001#
1772(10.9)
488(13.2)
0.0001#
Pre-Dalteparin
1(0.0)
647(13.8)
382(7.5)
330(9.0)
<0.0001#
1090(6.7)
270(7.3)
0.292#
Non-paused ASA
4(0.1)
1263(2.7)
2286(44.7)
2971(81.2)
<0.0001#
5391(33.2)
1133(30.6)
0.0001#
Non-paused APT
2(0.0)
549(11.7)
468(9.2)
201(5.5)
<0.0001#
959(5.9)
261(7.0)
0.009#
Table 1: Demographics and preoperative factors of patient cohort divided on time periods and gender. Comorbidity is EuroSCORE I minus age, sex, and surgery factors. Statistics: #) Χ2-test, all other ANOVA/Students independent t-test. ASA=Acetylsalicylic Acid; APT=Anti Platelet Therapy.
Overall, the yearly number of procedures declined from 1,534 in 2002 to 668 in 2018, although with a prominent up and down pattern (Figure 3), likely explained by changing surgical policies and the initiation and increase of PCI in the early years and transcutaneous aortic valve implantation late first decade leading to more single CABG instead of previous valve and CABG combinations.
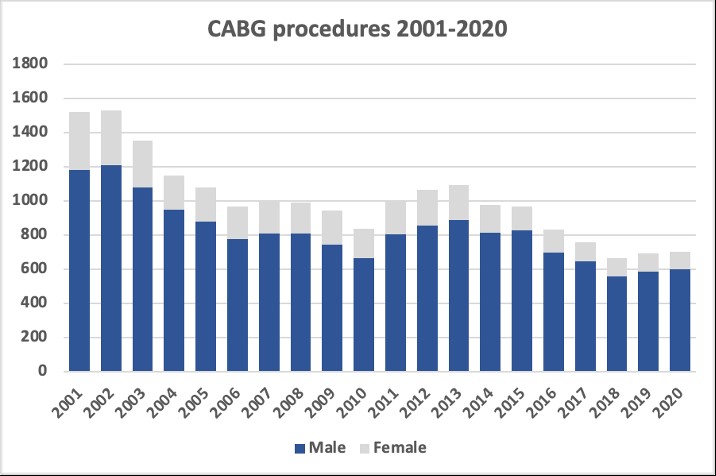
Figure 3: Included procedures divided on gender and year.
The grafting details in CABG and combined procedures are given in table 2. In general, more vessels seemed affected in men than in females (4.75 coronary vessel vs 4.40) and the mean stenosis was marginally higher as well. Males more often received LIMA but difference in the use of RIMA or BIMA was seen. Further, females have significantly higher fraction of low diameter coronary vessels (<1.5 mm) on the left side.
Graft details
Male
Female
p-value
CAG = 90-days before surgery
Number of vessels evaluated
4.75±1.86
4.40±1.71
<0.001*
Mean stenoses of vessels
80.1±17.1
79.2±17.5
0.007*
Number anastomosis
Number peripheral
2,75
2,46
<0.001
Number central
1,14
1,07
<0.001
Sequential ratio
2,42
2,29
Use of LIMA/RIMA
LIMA
90,9%
84,8%
<0.0001
RIMA
3,8%
3,7%
0.936
Both
3,2%
2,7%
0.055
Vessel diameter =1.5 mm
Left side vessels
25,8%
32,6%
<0.0001
Right side vessels
35,7%
37,1%
0.193
Table 2: Population background survival divided on 5-year periods and gender. Survival curves based on one year mortality of the actual ages (15-99 years; Data from Danish Statistics). https://www.dst.dk/en/
The registered complications were generally decreased over the decades except re-exploration due to bleeding and stroke higher in females (Table 3). Stroke, perioperative myocardial infarction, postoperative new dialysis, high volume of blood transfusion and long time in ICU declined during the observation period, while treatment with vasoconstrictors increased. Treatment with inotropes, re-exploration due to bleeding and ventricular fibrillation show differences between periods, but without a clear trend. A new CAG in the postoperative period, indicating recurrence of symptoms or new coronary disease, was fluctuating over time, but was in general significantly higher in men than females (Table 3).
Complication
Periods
Gender
2001-2005
2006-2010
2011-2015
2016-2020
p-value
Male
Female
p-value
Re-exploration
6,3%
5,3%
5,0%
5,7%
0.011
6,6%
6,4%
0.242
Stroke
1,6%
1,4%
1,2%
1,2%
0.229
1,5%
1,8%
0.059
AMI
6,3%
4,8%
4,0%
2,4%
<0.0001
4,0%
4,9%
<0.0001
New Dialysis
1,9%
1,6%
1,2%
0,9%
<0.0001
1,8%
2,5%
0.023
Constrictors
9,2%
24,6%
41,6%
62,6%
<0.0001
34,2%
38,1%
<0.014
Inotropes
9,1%
16,9%
14,8%
10,3%
<0.0001
14,5%
18,4%
<0.0001
Long ICU
7,6%
6,6%
3,5%
3,4%
<0.0001
5,8%
8,0%
<0.0001
VT/VF
2,1%
1,2%
1,0%
0,8%
<0.0001
0,7%
0,9%
0.005
RBC =7 units
3,4%
3,2%
2,0%
1,0%
<0.0001
2,7%
4,4%
<0.0001
CAG =30-days
5,2%
10,2%
11,2%
7,5%
<0.0001
8,7%
7,8%
0.0001
CAG =1-year
19,4%
30,0%
23,6%
17,4%
<0.0001
23,6%
20,2%
<0.0001
Table 3: Per- and postoperative complications. All statistics Χ2-test. AMI=Acute Myocardial Infarction; ICU=Intensive Care Unit; VF/VT=Ventricular Fibrillation/Tachycardia; RBC=Red Blood Cells.
The study group mortality declined during the 20-year period. Overall, the 1- year mortality declined 63.6 % and the 5-year mortality was reduced by 41.1% from the first to the last 5-year period. However, although narrowing in the last period, the short-term study group mortality was considerable higher than the background population mortality (Figure 4). The decrease in study patients correlated population mortality was greater than the public tables and readily explained by the changes in age patterns. Although the average age is relatively constant around 65-67 years, the number of especially women older than 80 years at surgery, were in the last period only 3.1% of the patients compared to 14.8% in the first period. For men this was more constant being 2.5% and 3.3% respectively. Further, the study group mortality was, except for the last period, statistically significant higher in females, in contrasts with the population, where mortality is higher in males than in females at all time points. Following, the fall in the study group mortality were more pronounced in females than in males. When evaluating the longer perspective, it seems that study group and population survival is almost balanced at the 5-year time point in males, while female mortality is somewhat higher even after 10 years compared to background population (Figure 5). Thus, male CABG patients had a better survival than the populations after just four years, while females never improve their survival to the level of the background population. The tendency with differences between the genders might be due to the general longer living time in females increasing the differences in older ages. However, the difference between genders among the study group and population survival after 10 year is remarkable being 69.3% vs 63.8% in men and 64.3% vs 68.8% in females.

Figure 4: Actual and expected 1- and 5-year mortality divided on 5-year time periods and gender. Statistically significant difference both in periods and gender (P<0.001, 2-way ANOVA). Insignificant actual mortality between gender in 2016-2020 (1-year, P=0.098 and 5-year, P=0.299; Independent samples t-test). Actual mortality in men is lower than population 2016-2020 (P<0.01; Independent samples t-test).
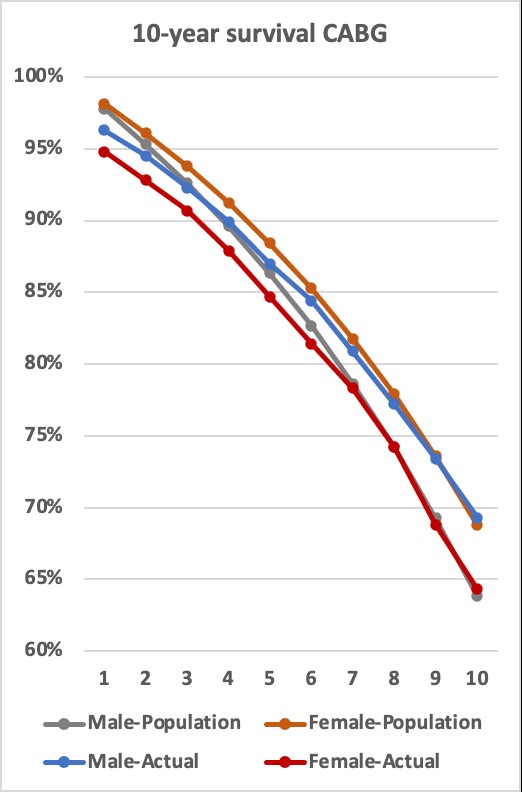
Figure 5: Actual and population 10-year survival. Major difference 1 year is in hospital/30 day’s mortality. Women actual survival never approach population survival in 10 years period. Males catch up with background population four years after surgery, while females do not reach background survival rates.
Detailed analysis revealed some differences when introducing procedure type, comorbidity, and perioperative complications (Figure 6). In general, both 1-year and 5-year mortality was higher for women. The comorbidity has a tremendous impact on the study group mortality as patient without comorbidity showed lower actual 1- and 5-year mortality in both male and females compared to population mortality. Further, males with low comorbidity showed marginally lower actual mortality while all other comorbidity groups showed higher actual mortality.
The mortality was significantly higher with just one perioperative complication and was extremely high with three or more perioperative complications, being 56.7% (1-year) and 65.2% (5-year). There was no difference in study group mortality between the sexes if two or more perioperative complications were present (Figure 6).
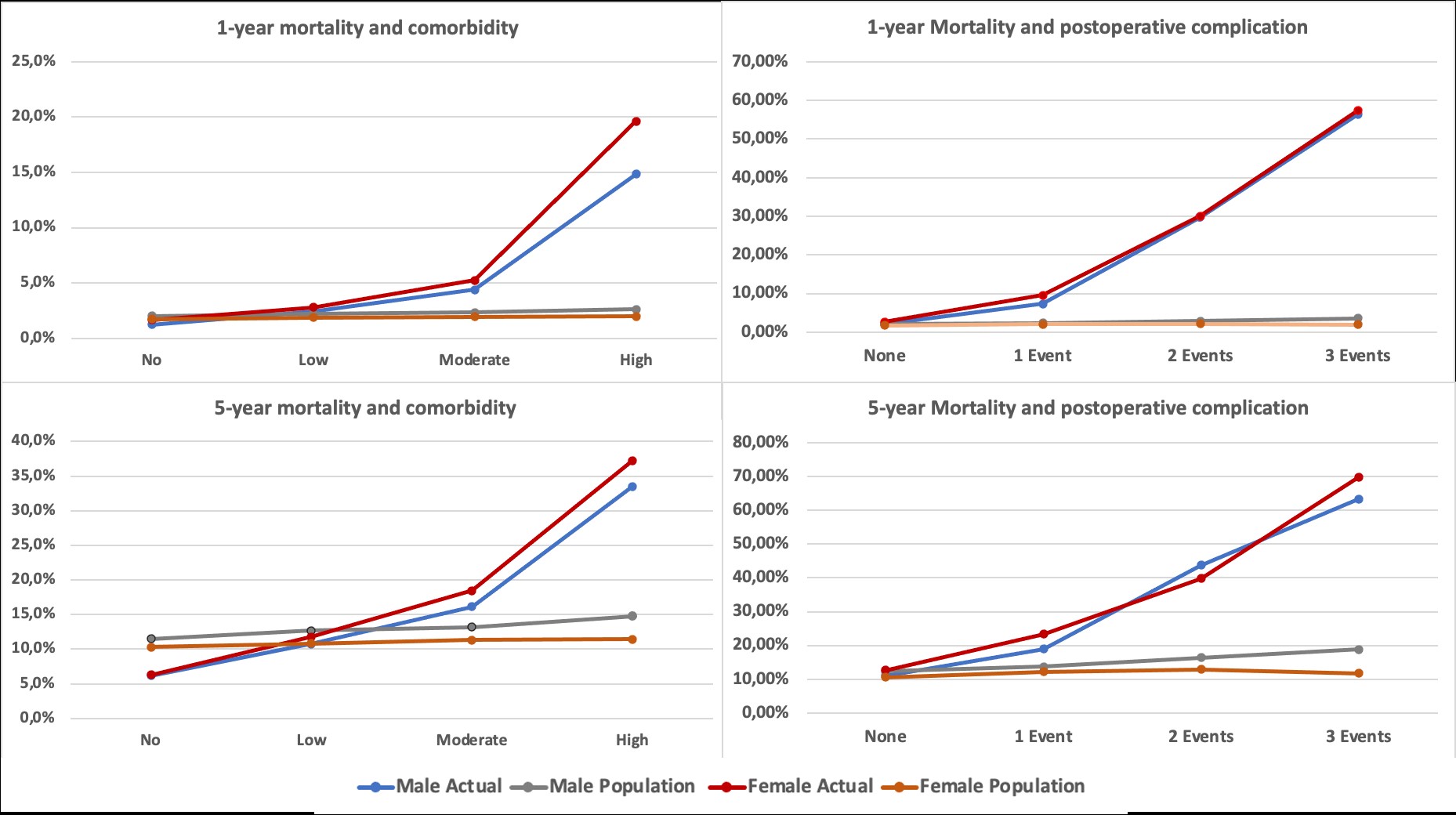
Figure 6: Actual and population 1- and 5-year mortality divided on gender and comorbidity (Left panel) and postoperative complications (Right panel). Actual 1- and 5-year mortality were lower than the background population in both gender without comorbidity and for men with low comorbidity. In all other comorbidity- groups the population background mortality was lower than the actual mortality. Actual 1- and 5-year mortality was marginally lower than the background population in males without complications.
Discussion
In this multicentre study, the perioperative data of almost 20,000 CABGs performed between 2001 and 2020 was analysed with focus on survival in relation to gender and further compared to the background population.
The most important findings were that females had somewhat more complications and a poorer short-term as well as long-term survival than males. Further, readily explained primarily by mortality in the near vicinity of surgery, the mortality of study patients was considerable higher than the background population in the first years after surgery. However, the gap narrowed during the following years and the actual male survival in the study patients surpassed the population survival after 4 years. On the contrary, compared to the background population, females undergoing CABG never reach the background population mortality.
Higher incidence of immediate postoperative complications, such as prolonged ICU stay, renal failure, need of inotropes, vasoconstrictors, and blood transfusions, as seen in the females in our study may suggest more and severe preoperative comorbidities such as compromised renal and lung function, severe atherosclerotic arteries, infarcted myocardium with poor ventricular function and severe diabetes.
Overall, the risk scores were higher in females primarily due to the female sex and a marginally higher age. Further, it is noted that, females in our study showed marginally higher basic comorbidity scores and in fact, fewer women got operated for CABG than men, suggesting lower incidence of coronary artery disease.
However, similar to observation in the previous studies [20-21], Danish females needed more complicated and non-elective surgeries than men, which may be responsible for some of the poorer outcomes reported. This may agree with the understanding that cardiovascular disease is recognized later in female and may lead to delays in investigation and subsequent treatment [22] as females are more likely to present with different symptoms to those thought of as “typical” [23] of cardiovascular disease. However, we also noted that the previously reported great difference in age at surgery has been decreased over the last decades but is still median 4 years in this study and 3 in the last 5-year period.
An additional explanation for the higher incidence of post operative complications may be derived from the observations presented in the British patient register study [22] which showed female sex as a risk factor for worse outcomes following both CABG and valve surgery. Authors speculate this to be related to the more challenging anatomy of female patients, such as smaller coronary arteries for grafting, narrower conduits, more diffuse pattern of coronary disease in addition to implantation of smaller sizes of valves, increasing the risk of patient-prosthesis-mismatch [21,24]. One of the same studies further suggested that sex-related differences in operative strategy decisions and techniques may explain sex-related differences in cardiac surgery outcomes e.g. a higher proportion of males compared with females received LIMA, RIMA, or BIMA grafting [25]. Similar to these findings, LIMA use in our study was less among females, despite the fact that, females showed higher fraction of narrowed, although without clinically significant blockages, left coronary arteries (Table 2), which may suggest that females may get predisposed to suboptimal myocardial revascularisation [26]. Similar observations are echoed in the United States STS data, from 2011 to 2019, showing that females are less likely to receive a LIMA to left anterior descending artery anastomosis [27]. However, as Denmark has uniform national cardiac surgery protocols, the difference in choice of conduit cannot be attributed to the differences in operative strategy decisions and techniques.
While exploring the etiology of higher postoperative RBC requirement midst females despite the benefits of procoagulant effect of estrogen [28-29], it was understood that mean age of females in the study was 74 years which indicate post-menopausal population where the above-mentioned protection of estrogen may not be present. Irrespective of higher bleeding, interestingly, there was no difference in the incidence of re-explorations for bleeding which along with longer stay in ICU suggest absence of the major indications of re explorations such as acute, profuse, and hemodynamic disturbing bleeding. This may suggest that females may have tendency for prolonged slow surgical blood loss through drains without creating hemodynamic disturbances and need for reexploration.
The findings that, females have more immediate post operative complications, longer ICU stay, higher RBC requirement itself partially explain higher incidence of short-term mortality. Besides the smaller coronaries, the approach of females in postoperative rehabilitation may have a major role in the long-term mortality. Cardiac rehabilitation participation was associated with a 32% risk reduction in all-cause mortality, and this benefit was independent of sex, age, socioeconomic status, and comorbidity [30]. It is observed that, coping with a cardiac event, women tend to minimize or neglect the impact of their health situation and avoid burdening their social contacts. A low attendance was also observed by women, giving the impression that women are less motivated and therefore less compliant towards cardiac rehabilitation [31]. Further, after a first cardiac event, women report greater psychological distress and lower self-efficacy and self-esteem. In addition, older age, lower exercise levels and reduced functional capacity or co-morbid conditions such as osteoporosis and urinary incontinence are barriers to physical activities in women with IHD [32]. The observation of difference in mortality in the study group and the background population may encourage us to have the discussion on benefits of cardiac interventions. Apart from relief from symptoms, cardiac surgeries are expected to offer long-term survival, not better than but at least similar to the background population. In contrast to the expectations, it was observed that the study females at all times had mortality higher than the background population, while men seemed to catch up after 4-5 years. The understanding that, surgical interventions apart from imparting trauma, may add or aggravate the comorbidities and in majority of situations have no role in reversal of the native disease, may partially explain the differences. Thus, the role of progression of the old and new comorbidities along with advancement of native disease and its impact on vital organs in the long-term survival cannot be denied. Further, most cardiac disease has their origin in patients´ lifestyle and similar to development of new cardiac disease, changes in the lifestyle may have positive impact on the progression of the native disease [33-34]. Over the last few decades, undoubtedly, the awareness of importance of modification of lifestyle has increased exponentially. As the impact of lifestyle modification is slow and gradual, the benefits on survival may likewise appear slowly. This effect may be seen in the equalization of mortality in men in the study with the population. The missed improved survival in the female study group, or at least being resembling the background population, may again be the reflection of delayed restitution and different approach in cardiac rehabilitation.
Strengths and Limitations
The authors declare full access to all registered data in the WDHR and accountability for data integrity and analysis.
The primary strengths of this study are the use of mandatory and obligatory prospectively reported data from a well-established uptake area and a database used by all institutions. The large cohort with detailed and complete follow-up data on all patients undergoing CABG surgery during more than 2 decades allows robust estimations of patients, results, and adverse events.
However, the retrospective nature of the study has inherent bias and carries possible confounders, but since registrations of all procedures are mandatory and all included patients and outcomes can be accounted for, it reduces the effect of some of the mentioned challenges. Nevertheless, our study has intrinsic limitations, as we cannot discard the non-randomized nature and that the additional effects of missing covariates and the lack of randomization, potentially increase the risk of confounding.
The surgical and anaesthesiological practice and policies have changed over the observation time, and diverse speed in implementations of innovations and new research potentially could have influenced indications and treatments, but the treatment in Denmark is generally very uniform, and due to the education system, all doctors are trained in more than one center.
Conclusion
Females have a substantial higher mortality than males after CABG compared to the background population. Males seem to catch up with population mortality 4-5 years after surgery, while females continue to have a lover survival than the background population.
Author Statements
Sources of Funding
Except support from authors clinics, no external funding.
Disclosures
The authors have nothing to disclose.
References
- World Health Organization. Top 10 causes of death worldwide Geneva: WHO; 2017.
- Millett ERC, Peters SAE, Woodward M. Sex differences in risk factors for myocardial infarction: cohort study of UK Biobank participants. BMJ. 2018; 363: k4247.
- Henry S, Bond R, Rosen S, Grines C, Mieres J. Challenges in cardiovascular risk prediction and stratification in women. Cardiovasc Innov Appl. 2019; 3: 329-48.
- Groepenhoff F, Bots SH, Kessler EL, Sickinghe AA, Eikendal ALM, Leiner T, et al. Sex-specific aspects in the pathophysiology and imaging of coronary macro- and microvascular disease. J Cardiovasc Transl Res. 2020; 13: 39-46.
- Haider A, Bengs S, Luu J, Osto E, Siller-Matula JM, Muka T, et al. Sex and gender in cardiovascular medicine: presentation and outcomes of acute coronary syndrome. Eur Heart J. 2020; 41: 1328-36.
- Peters SAE, Huxley RR, Woodward M. Diabetes as risk factor for incident coronary heart disease in women compared with men: a systematic review and meta-analysis of 64 cohorts including 858,507 individuals and 28,203 coronary events. Diabetologia. 2014; 57: 1542-51.
- Huxley RR, Woodward M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: a systematic review and meta-analysis of prospective cohort studies. Lancet. 2011; 378: 1297-305.
- Statistics Denmark. Available from: https://www.statistikbanken.dk/statbank5a/default.asp?w=1436.
- Joensen AM, Joergensen T, Lundbye-Christensen S, Johansen MB, Guzman-Castillo M, Bandosz P, et al. Explaining trends in coronary heart disease mortality in different socioeconomic groups in Denmark 1991-2007 using the IMPACTSEC model. PLOS ONE. 2018; 13: e0194793.
- Jensen J. Gender differences in ischemic heart disease. Ugeskr Laeger. 2007; 169: 2435-7.
- Rosengren A, Wallentin L, Simoons M, Gitt AK, Behar S, Battler A, et al. Age, clinical presentation, and outcome of acute coronary syndromes in the Euroheart acute coronary syndrome survey. Eur Heart J. 2006; 27: 789-95.
- Roques F, Nashef SA, Michel P, Gauducheau E, de Vincentiis C, Baudet E, et al. Risk factors and outcome in European cardiac surgery: analysis of the EuroSCORE multinational database of 19030 patients. Eur J Cardiothorac Surg. 1999; 15: 816-22.
- Nashef SAM, Roques F, Sharples LD, Nilsson J, Smith C, Goldstone AR, et al. EuroSCORE II. Eur J Cardiothorac Surg. 2012; 41: 734-44.
- Mølstad P, Moer R, Rødevand O. Long-term survival after coronary bypass surgery and percutaneous coronary intervention. Open Heart. 2016; 3: e000489.
- Weintraub WS, Clements SD Jr, Crisco LvT. Guyton RA, Craver JM, Jones EL, et al. Twenty-Year survival after coronary artery surgery. An institutional perspective from Emory University. Circulation 2003; 107: 1271-7.
- Adelborg K, Horváth-Puhó E, Schmidt M, Munch T, Pedersen L, Nielsen PH, et al. Thirty-year mortality after coronary artery bypass graft surgery. A Danish nationwide population-based cohort study. Circ Cardiovasc Qual Outcomes. 2017; 10: e002708.
- Rexius H, Brandrup-Wognsen G, Ekroth R, Odén A. Does coronary artery bypass surgery improve survival? Scand Cardiovasc J. 2012; 46: 269-77.
- Schmidt M, Maeng M, Madsen M, Sørensen HT, Jensen LO, Jakobsen CJ. The Western Denmark heart registry: its influence on cardiovascular Patient Care. J Am Coll Cardiol. 2018; 71: 1259-72.
- Statistics Denmarks. [Befolkning og doedsfald 2020]. Available from: https://www.dst.dk/en/Statistik/emner/borgere/befolkning/doedsfald.
- Dixon LK, Dimagli A, Di Tommaso E, Sinha S, Fudulu DP, Sandhu M, et al. Females have an increased risk of short-term mortality after cardiac surgery compared to males: insights from a national database. J Card Surg. 2022; 37: 3507-19.
- Dalén M, Nielsen S, Ivert T, Holzmann MJ, Sartipy U. Coronary artery bypass grafting in women 50 years or younger. J Am Heart Assoc. 2019; 8: e013211.
- Haider A, Bengs S, Luu J, Osto E, Siller-Matula JM, Muka T, et al. Sex and gender in cardiovascular medicine: presentation and outcomes of acute coronary syndrome. Eur Heart J. 2020; 41: 1328-36.
- Parvand M, Rayner-Hartley E, Sedlak T. Recent developments in sex-related differences in presentation, prognosis, and management of coronary artery disease. Can J Cardiol. 2018; 34: 390-9.
- Urbanowicz T, Michalak M, Olasinska-Wisniewska A, Haneya A, Straburzynska-Migaj E, Bocianski M, et al. Gender differences in coronary artery diameters and survival results after off-pump coronary artery bypass (OPCAB) procedures. J Thorac Dis. 2021; 13: 2867-73.
- Gaudino M, Samadashvili Z, Hameed I, Chikwe J, Girardi LN, Hannan EL. Differences in long-term outcomes after coronary artery bypass grafting using single vs multiple arterial grafts and the association with sex. JAMA Cardiol. 2020; 6: 401-9.
- Hessian R, Jabagi H, Ngu JMC, Rubens FD. Coronary surgery in women and the challenges we face. Can J Cardiol. 2018; 34: 413-21.
- Jawitz OK, Lawton JS, Thibault D, O’Brien S, Higgins RSD, Schena S, et al. Sex differences in coronary artery bypass grafting techniques: a society of thoracic surgeons database analysis. Ann Thorac Surg. 2022; 113: 1979-88.
- Ambrus JL, Schimert G, Lajos TZ, Ambrus CM, Mink IB, Lassman HB et al. Effect of antifibrinolytic agents and estrogens on blood loss and blood coagulation factors during open heart surgery. J Med. 1971; 2: 65-81.
- Saxena A, Dinh D, Smith JA, Shardey G, Reid CM, Newcomb AE. Sex differences in outcomes following isolated coronary artery bypass graft surgery in Australian patients: analysis of the Australasian Society of Cardiac and Thoracic Surgeons cardiac surgery database. Eur J Cardiothorac Surg. 2012; 41: 755-62.
- Eijsvogels TMH, Maessen MFH, Bakker EA, Meindersma EP, van Gorp N, Pijnenburg N, et al. Association of cardiac rehabilitation with all-cause mortality among patients with cardiovascular disease in the Netherlands. JAMA Netw Open. 2020; 3: e2011686.
- Oosenbrug E, Marinho RP, Zhang J, Marzolini S, Colella TJ, Pakosh M, et al. Sex differences in cardiac rehabilitation adherence: A meta-analysis. Can J Cardiol. 2016; 32: 1316-24.
- Smith JR, Thomas RJ, Bonikowske AR, Hammer SM, Olson TP. Sex differences in cardiac rehabilitation outcomes. Circ Res. 2022; 130: 552-65.
- Rizzuto D, Orsini N, Qiu C, Wang HX, Fratiglioni L. Lifestyle, social factors, and survival after age 75: population based study. BMJ. 2012; 345: e5568.
- Fernández-Ballesteros R, Valeriano-Lorenzo E, Sánchez-Izquierdo M, Botella J. Behavioral lifestyles and survival: A meta-analysis. Front Psychol. 2021; 12: 786491.