
Research Article
Thromb Haemost Res. 2022; 6(3): 1085.
Differences in Assessments of Total Burn Surface Area Involving Children Transferred To A Burn Center for Treatment – Experience In Southern Brazil
Saviatto LG, Picasky JP, Azevedo BBS, Feijó RS, Camacho JG, Soares FF and Pereima MJL*
Burn unit, Joana de Gusmão Children Hospital, Department of Pediatric, Federal University of Santa Catarina, Florianópolis, Brazil
*Corresponding author: Mauricio José Lopes Pereima Departament of Pediatric, Centro de Ciências da Saúde Universidade Federal de Santa Catarina, Campus Universitário David Ferreira Lima, Trindade - CEP 88040-900 Florianopolis - Santa Catarina - Brazil
Received: November 08, 2022; Accepted: December 17, 2022; Published: December 23, 2022
Abstract
Purpose: To analyze discrepancies between the evaluation of total body surface area (TBSA) of burn injuries involving children performed by clinicians at hospitals and clinics in southern Brazil before patients are transferred to a Burn Care Unit (BU) and the same evaluation by trained burn specialists, in order to determine the accuracy of burn size estimation and to evaluate clinical data to inform whether efforts to increase knowledge are warranted to optimize early management and treatment of burned pediatric patients.
Methods: This is an observational study in which data was analyzed involving burn patients transferred from regional hospitals and clinics for admission to Joana de Gusmão Children’s Hospital, located in the city of Florianópolis in southern Brazil, that maintains a BU for referral of pediatric patients. The analysis consists of comparisons between the estimated values of TBSA of the burn obtained from the “Transferred burnt patient form” completed by the referring clinician and values registered in patient records upon arrival at the BU. In addition, other quantitative and qualitative data, such as burn mechanism patient age, and whether resuscitation with intravenous (IV) fluids occurred, were collected to further inform management and treatment of the injuries.
Results: At the early assessment, there was overestimation of TBSA burned in 76.4% of patients (n = 39), 32 of those had a TBSA of less than 15%, and the mean TBSA estimate was 291% higher (p-value 0.0001). The 1-4 age group represented the largest group of patients, 56.4% (n =29), and the most common mechanism of burn was due to heated water in 60.8% (n=31) of the cases. There was correlation (p-value 0.014) between increased length of hospitalization and burn mechanism when the burn was caused by direct contact with fire or electric shock which resulted in patients staying for 26 ± 9.35 days. In addition, 66.7% of patients included in this study had been administered IV fluids at the city of origin prior to arriving at the children’s BU.
Conclusion: When the estimate of the TBSA of the burn obtained by non-specialists, was compared to the estimate after admission to a specialized burn unit, there was an overestimation in most cases and this has the potential to lead to mismanagement of pediatric burn patients.
Keywords: Burn wound; Children; Burn unit; Body surface area
Introduction
In Brazil, burn injury represents a major concern in public health with an incidence of more than 1 million cases per year and, of those, 40 thousand require hospitalization and children account for two thirds of the cases [1,2]. In the United States, burn injury, traffic accidents, drowning, and suffocation represent the four most common causes of unintentional injury, which is the major cause of death category for children ages 1 through 14 years. Burn injury is defined as trauma to skin layers and adjacent tissue caused by a variety of energy sources such as electrical, chemical, thermal or radioactive. Therefore, the rupture of skin integrity means the loss of a protective barrier that compromises thermal control and hydro electrolytic homeostasis [4,5].
In order to assess the patient according to burn severity to determine patient management and prognosis, specific variables must be considered such as depth of the burn injury, patient age, burn mechanism, and the Total Body Surface Area (TBSA) affected by the injury [6]. The TBSA estimation has great relevance because it allows categorizing the patient according to the extent of the burn [7,8]. The TBSA of partial and full thickness burns can be estimated using a variety of methods. The earliest evidence of this approach was found to occur in the19th century with use of the Berkow estimation which is considered a precursor to two rules widely used nowadays; the “rule of palm” and “Wallace’s rule of nines.” [9] This latter tool identifies anatomical regions as multiples of 9 of TBSA affected by a burn and, like the “rule of palm”, uses a parameter that the surface of the palm of the hand represents 1% of TBSA [9,10]. Both of these methods are considered to be fatly, as they can incorrectly estimate TBSA burned especially if the patient is overweight or is a pediatric patient [10]. The Lund and Browder method is recognized as the most accurate for use in the pediatric population, because it considers the age of the patient when estimating TBSA [9]. Besides these methods, new technology allows the TBSA burn estimation to be performed using a smartphone Application (app) [9,10].
An adequate TBSA evaluation of a burn is the critical starting point that leads to correct management of the patient because it is crucial for calculating the volume of intravenous fluid to administer in resuscitation therapy, a treatment proven to impact survival rates [11]. Incorrect evaluation of the TBSA burned can be harmful and result in serious complications to those with more than 20% of body surface compromised by burnt tissue [12,13]. An underestimation of the TBSA can lead to hypovolemia and, as a consequence, kidney failure, acute tubular necrosis, bacterial translocation from the gastrointestinal tract in intestinal ischemia, and burn deepening at Jackson’s stasis zone [11,14,15]. In contrast, over hydration, when it exceeds the value calculated through Parkland’s formula, may cause a phenomenon described by Pruitt as “fluid creep” that originates from edema in burnt and non burnt tissue. It may also cause compartmental abdominal syndrome or deepening of the burn with compromised tissue perfusion and infections [16]. Literature suggests that overestimations of the TBSA burn are more common than underestimations, because calculations require expert knowledge of burn injuries [10,13]. Discrepancies greater than 2 to 3% may result in increased mortality rates [10,14]. Furthermore, although patients given an underestimation of the TBSA burn might receive inadequate fluid resuscitation before transfer to a BU, patients given an overestimation of TBSA burn could have been managed at the original medical facility instead of overloading the BU center. with an unnecessary transfer [17].
The purpose is analyze discrepancies between the evaluation of the Total Body Surface Area (TBSA) of burn injuries involving children performed by clinicians at hospitals and clinics in southern Brazil before patients are transferred to a Burn Care Unit (BU) and the same evaluation by trained burn specialists, in order to determine the accuracy of burn size estimation and to evaluate clinical data, such as medical interventions and length of hospitalization, to inform whether efforts to increase knowledge are warranted to optimize early management and treatment of burned pediatric patients.
Methods
This is an observational study in which data collected over a period of eight months was analyzed involving burn patients transferred from regional hospitals and clinics for admission to the Burn Care Unit (BU) at Joana de Gusmão Children’s Hospital (HIJG) .The hospital serves as referral center for pediatric patients for the state of Santa Catarina in southern Brazil and is located in the state’s capital, Florianópolis, with an estimated population of 7,338,473. [18] The analysis consists of comparison between the values of TBSA of the burn obtained in the form “Transferred burnt patient form” (Figure 1) completed by the referring clinician and values registered in patient records upon arrival at the BU. In addition, other quantitative and qualitative data, such as burn mechanism, patient age, and whether resuscitation with intravenous (IV) fluids occurred, were collected to further inform management and treatment of the injuries. The whole process was grounded in the guidelines established by the National Health Council of Health Ministry of Brazil for research regarding human beings [19]. This guideline provides rules and standards in bioethics, granting rights and duties concerning persons involved in scientific research and its outcomes [20].
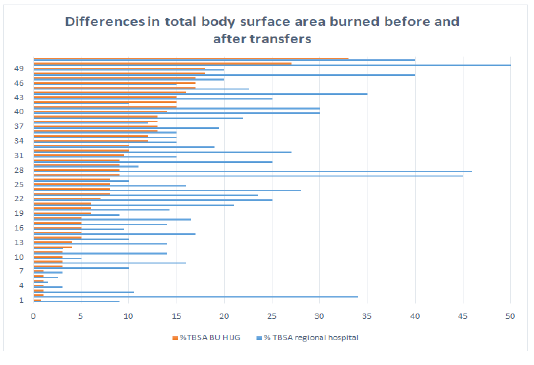
Figure 1: Estimations of %TBSA of burnt pediatric patients transferred
to Joana de Gusmão children´s hospital burn unit and differences
in %TBSA before and after transfers of the whole sample.
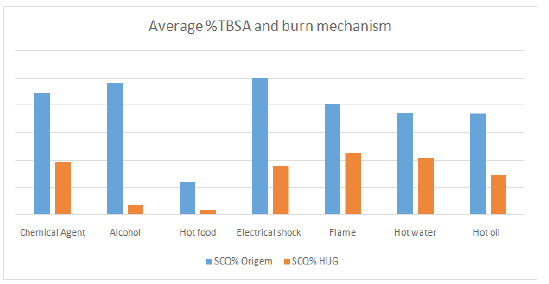
Figure 2: Contrast between estimations of TBSA before and after
being transferred to the burn unit, according to burn mechanism.
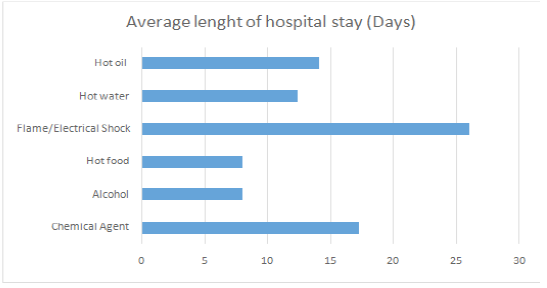
Figure 3: Average length of hospital stay branched by burn mechanism.
In addition to analysis of quantitative and qualitative data involving patient demographics and medical interventions, statistical analysis was performed between the value of TBSA of the burn obtained before and after patients were transferred to the referral BU. When the error of the initial TBSA estimation was greater than 25% of the TBSA assessment by experts, it was considered an overestimation. The original estimation was within an acceptable estimate when the error range was 25% (from -25% to +25%). Statistical analysis was obtained using Epi-info software through an ANOVA test when comparing more than two groups and using a T test when comparing only two. A p-value of less than 0.05 was used to determine statistical significance.
To allow meaningful statistical analysis, the only patient with a TBSA percentage error of less than 25% was placed amongst those considered with an adequate estimation. For the same reason, the only patient in which the burn mechanism was electrical shock was added to the group in which the burn mechanism was direct fire burn.
Results
Data from 72 patients were collected; however, 21 were excluded because the transfer form was not completed in entirety. Therefore, the sample consists of 51 patients in which 40 (78, 4%) presented with a TBSA estimation of the burn at less than 15% and 11 (21, 6%) had a TBSA of more than 15%. The percentage of error of the TBSA estimation before transfer to the BU averaged 47.8%, (9.04 ± 9.59%).
Of 51 patients sampled during the study period, over half of them were between 1 and 4 years old (56.9% n=29), 11 were less than 1 year old (21.6%) and, in this latter group, the estimated average difference of TBSA was 13.6 ± 11.9% with an overestimation of the TBSA at 145%. Four patients (7.8%) were in the 5 through 9-year-oldgroup and there was a total of seven patients (13.7%) between 10 to14 years old.
Regarding burn mechanism previously established by cited authors, hot water had the largest number of “victims” being responsible for 60.8% (n= 31) of patient injuries, followed by hot oil (13.7%, n= 7), fire and electric shock (9.8%, n= 5), and chemical agents (7.8%, n=4). Alcohol and hot food, together, account for less than 10% of the sample. The average difference of TBSA estimated at regional hospitals and clinics, when compared to the one obtained at HIJG, was 8.3 ± 8.1% for those in which the burn mechanism was scalding by hot water, with an average percentage error of 96.0% (p-value <0.05). Of those who were burnt by alcohol, the average difference of the TBSA estimate was 22 ± 15.5%.
The majority of patients were hospitalized for a period of 15 to 28 days (n=21, 41.2%, p-value 0.013), while only 3 patients (5.9%) stayed for less than2 days or more than 28 days. The hospitalization at HIJG lasted 3 to 7 days for eight patients (15.7%) and 8 to 14 days for 16 patients (31.3%). For those whose stay lasted 15 to 28 days, the estimate of the TBSA was 9.7 ± 11.1% had an average error of 82% (p-value 0.316).
Nineteen (37.2%) of 51 patients were only treated with fluid resuscitation or dressings. The remaining 62.7% (n=32) had also had either facial laser, skin grafting, and/or transfusion with red bloodcells. All of the patients that required red cell blood transfusions had been through dermoepidermic skin grafting (n=11, 21.5%), and one (1.9%) had received all three interventions as shown in (Table 3). Of all the patients, one was admitted to the Intensive Care Unit (ICU) due to electrolytedys function with clinical development. Before transfer from the initial hospital or clinic, 34 (66.6%) patients were given IV fluids, as described on the form requested, although not all of the participants claimed using Parkland’s formula to calculate volume. Data regarding the IV fluid regimen administered before and at HIJG were not collected for this study, as these data were not provided in most cases in the patient transfer documents.
Variable
n (%)
TBSA regional hospital %
TBSA BU HIJG %
Estimative difference
Percentage error %
p
%TBSA, n (%)
0.8389
<15%
40 (78.4)
16.40
6.61
9.78 ± 9.24
148
=15%
11 (21.6)
27.95
18.91
9.04 ± 9.59
47
Estimative before transfer, n (%)
0.0001
Overestimated
39 (76.4)
19.92
7.72
12.20 ± 8.96
291
Underestimated/adequate
12 (23.5)
15.50
14.25
1.25 ± 3.07
7.3
n, number
TBSA regional hospital%, Average estimation of total body surface area burned at the regional hospital.
TBSA BU HIJG %, Average estimation of total body surface area burned at Joana de Gusmão Children’s Hospital burn unit.
P, p value.
Table 1: Burnt patient distribution transferred to Joana de Gusmão Children’s Hospital, in the period between May of 2021 and January of 2022, according to burn extension in %, TBSA estimation at regional hospital in contrast to the one obtained at Burn Unit of HIJG.
Estimatives
Variable
n (%)
TBSA regional hospital %
TBSA BU HIJG %
Estimative difference
Percentage error %
p
Age group, n (%)
0.1026
<1year old
11(21.6%)
23.1
9.4
13.65 ± 11.9
145
1 – 4
29(56.9%)
16.9
8.2
8.14 ± 8.53
105
5 – 9
4(7.8%)
25.4
16.0
9.64 ± 6.54
59
10 – 14
7(13.7%)
15.8
7.1
9.25 ± 9.67
121
Burn mechanism, n (%)
0.0000
Chemical agent
4 (7.8)
22.25
9.75
12.50 ± 9.72
313
Alcohol
2 (3.9)
24.00
2.00
22.0 ± 15,5%
1100
Hot food
2 (3.9)
6.00
0.90
5.10 ± 4.38
612
Flame/Electric shock
5 (9.8)
21.25
10.90
10.30 ± 6.88
96
Hot water
31 (60.7)
18.68
10.39
8.29 ± 8.14
124
Hot oil
7 (13.7)
18.44
7.29
11.15 ± 13.39
161
Lenghtofstay, n (%)
0.3167
0 – 2
3 (5.9)
1517
7.67
7.50 ± 3.60
98
3 – 7
8 (15.7)
17.75
7.23
10.52 ± 6.79
146
8 –14
16 (31.3)
16.61
7.38
9.23 ± 9.62
125
15 –28
21 (41.2)
21.62
11.88
9.73 ± 11.10
82
> 28
3 (5.9)
18.67
8.00
10.66 ± 3.78
133
Total, n (%)
51 (100)
18.88
9.26
9.62 ± 9.22
104
n, number
TBSA regional hospital %, Average estimation of total body surface area burned at the regional hospital;
TBSA BU HIJG %, Average estimation of total body surface area burned at Joana de Gusmão Children’s Hospital burn unit;
P, p value.
Table 2: Distribution of burnt patients transferred to Joana de Gusmão Children´s Hospital, between May 2021 and January 2022, by TBSA estimation at regional hospital in contrast to the one obtained at Burn Unit of HIJG, according to age group, burn mechanism and length of hospital stay.
Estimatives
Variable
n (%)
TBSA regional hospital %
TBSA BU HIJG %
Variable
n (%)
TBSA regional hospital %
Intervention, n (%)
0.3803
Laser
8 (15.7)
16.79
5.13
11.66 ± 11.47
228
SkinGraft
10 (19.6)
13.80
10.40
3.40 ± 3.92
33
Redbloodcelltransfusion
0 (0.0)
--
--
--
--
Laser + SkinGraft
2 (3.9)
23.00
7.50
15.50 ± 0.70
207
Skin Graft + Red blood cell transfusion
11 (21.5)
24.45
12.36
13.65 ± 11.9
98
Laser + Skin Graft + Red blood cell transfusion
1(1.9)
15.00
13.00
2.00 ± 0.00
15
None
19(37.2)
19.00
8.59
10.40 ± 8.86
121
Total, n (%)
51 (100)
18.88
9.26
9.62 ± 9.22
228
n, number
TBSA regional hospital %, Average estimation of total body surface area burned at the regional hospital.
TBSA BU HIJG %, Average estimation of total body surface area burned at Joana de Gusmão Children’s Hospital burn unit;
P, p value
Table 3: Distribution of burnt patients transferred to Joana de Gusmão Children´s Hospital, between May 2021 and January 2022, by TBSA estimation at regional hospital in contrast to the one obtained at Burn Unit of HIJG, according to intervention.
Variables such as age, burn mechanism, difference between the TBSA estimations at regional hospitals (overestimation, adequate, and underestimation) and extent of the TBSA (less than 15% or equal and/or greater than 15%) were analyzed statistically with length of hospitalization to determine if there was significance. The results are available in table 4 showing that hospital stay was significantly related to burn mechanism, and the longest stay involved those burnt by fire and electric shock (26 ± 9.35 days, p-value 0.014), followed by chemical agents (17.25 ± 4.03 days), and lastly, hot oil, hot water, burnt food and alcohol with the shortest length of hospital stay (8.00 ± 0.00 days).
Variable
n (%)
Lenght of hospital stay (days)
P
Age group, n (%)
0.102
<1yearold
11(21.6%)
12.09 ± 7.13
1 – 4
29(56.9%)
12.82 ± 8.20
5 – 9
4(7.8%)
15.25 ± 7.41
10 – 14
7(13.7%)
21.28 ± 10.99
Burn mechanism, n (%)
0.0146
Chemical agent
4 (7.8)
17.25 ± 4.03
Alcohol
2 (3.9)
8.00 ± 0.00
Hot food
2 (3.9)
8.00 ± 5.65
Flame/ Electric shock
5 (9.8)
26.00 ± 9.35
Hot water
31 (60.7)
12.41 ± 7.64
Hot oil
7 (13.7)
14.14 ± 9.78
Estimative before transfer, n (%)
0.316
Overestimated
39 (76.4)
13.41 ± 9.16
Underestimated
1 (1.9)
12.00 ± 0.00
Adequate
11 (21.5)
16.50 ± 5.79
%TBSA, n (%)
0,240
<15%
40 (78.4)
13.27 ± 8.97
= 15%
11 (21,.)
16.72 ± 7.04
Total, n (%)
51 (100)
14.01 ± 8.64
n, number
P, p value.
Table 4: Distribution of burnt pediatric patients transferred to HIJG burn unit according to age group, burn mechanism, correctness of %TBSA estimation, and burn extension in %TBSA in regards of length of hospital stay.
Discussion
The evaluation of the TBSA of a burn has direct impact on the prognosis of burnt patients, especially in the pediatric population in which the ratio between body surface areas over body weight is greater when compared to adults, and small differences and delays in obtaining correct estimations may result. In poor out comes [14]. It is well published that the Parkland formula, that relates TBSA with weight and patient age, provides adequate accuracy to guide fluid resuscitation of a burnt patient and, at times, it has shown to be superior to the goal directed strategy which has a greater occurrence of “fluid creep” [11]. This phenomenon, a result of excessive fluid resuscitation, is responsible for complications such as anasarca, superior airway obstruction with the need for intubation, increased time to remain intubated, deepening of burnt areas, and compartmental abdominal syndrome [16]. Furthermore, it is known that excessive IV fluid infusion in the first 24 hours, that is higher than that calculated by Parkland’s formula, results in a cycle of subsequent over hydration during the following hours which exacerbates the negative effects of fluid creep [16,21].
When comparing the TBSA estimate obtained in regional hospitals and clinics with the one the BU of HIJG assessed, there was an overestimation in 76.4% of patients (n = 39), similar to the findings by Armstrong, et al. [22] with 77%. Of those with an exaggerated estimate of TBSA, 32 were in the group with less than 15% and that evaluation was an average 291% greater than the one given by specialists at the BU, with estimated difference of TBSA of 12.20 ± 8.96. The systematic review published by Brekke et al. [23], that included 28 studies, cites overestimation with an average involving more than 50% of the patients of the studies analyzed. In this research there was an adequate estimation of the TBSA of the burn in only 21.5% (n=11) of patients and one underestimation (1.9%). In those patients the average error was 7.3%. The rate of overestimation versus underestimation of TBSA in this study is 39:1.
Literature describes [9,24,25] that the error of TBSA estimation can be as high as 200% when comparing the numbers obtained by non-specialists before transfer to a BU and the estimates obtained at the burn center. This present study found an average of l difference of 104% more in the estimate made by non-specialists. It is mentioned in studies [22,26] that patient with burns of minor extent, at times less than 20%, and others less than 15%, are the most overestimated. Therefore, this study has shown that 82% of the 39 patients that had the TBSA exaggerated had burns of less than 15% of TBSA. The systematic review by Brekke et al. [22] corroborates our findings, showing a trend of overestimations in patients transferred to a burn unit and that the larger the extent of the burn, the less this phenomenon occurs.
In 2021, Armstrong et al. [27] used a sample of6 thousand pediatric patients and reported that the age group from 1 through 4 years old is responsible for nearly half of the hospitalizations due to burns in the United States (US). This present research agrees with those results whereby, of the 51 patients in our analysis, 56.9% (n=29) are included in that category. Older children, 10 to 14 years old, had the longest hospital stay, with an average of 21.2 ± 10.99 days, while patients less than 1 year of age had an average of 12.0 ± 7.13 days. The study by Armstrong et al. [27] reported that there was no statistical relevance in the difference of the length of hospitalization in relationship to different age groups (p-value > 0.05).
Regarding the other variables, the length of hospital stay was not statistically relevant to the difference in TBSA estimation, nor to the extent of TBSA (When the length of hospital stay was analyzed in relation to the causal agent of the burn, there was a relevant difference, with patients burned by fire and electrical shock staying longer in the hospital, with a mean stay of 26 ± 9.3 days (p-value 0.014). The epidemiological study by Armstrong et al. [27] shows this burn mechanism as one of those with longer hospital stays, after intentional burns, an object not evaluated in this study. In Dittrich, et al. [16] it was concluded that a hospital stay longer than 14 days, if associated with the occurrence of the “fluid creep” event, was related to infections and worse prognosis in these scenarios. The percentage error in the TBSA estimate was statistically relevant when in association with burn mechanism, although no data to corroborate this analysis was found in literature. Scalding, caused by hot water, is usually cited [27,28] as the major cause of burn injury in children, which is also demonstrated in this study. The boiling of water is present in several daily activities, and as the major cause of burn injury in the pediatric population, it aligns with the statistics of deaths by accidental cause, that brings a warning sign to the population in general.
The type of procedure performed did not show significant relevance when compared to the percentage error in TBSA estimation. In Daniels, et al. [11] it was concluded that permissive hypovolemia - when hydration is performed at lower, though still safe, volumes than those established by the formula developed by Baxter - represents fewer interventions and procedures performed, and also shows as a result fewer unfavorable outcomes, with lower mortality rates compared to patients with over hydration. [11,16] The error in TBSA estimation is closely related to fluid resuscitation [14] and 66.7% of patients included in this study were subjected to IV fluid replacement before transfer to the BU. Consider that 76.4% had their TBSA estimated with, on average, 291% more than what is considered to be correct, it is possible to affirm the occurrence of over hydration and fluid creep even before transfer. As exposed in research performed by Daniels, et al. [11], 70% of institutions use the Parkland formula, however, despite this, 55% to 100% of the patients receive increased volumes of fluid resuscitation when correctly evaluated. Similar information is described in Shah, et al. [21] with 69% of the burn unit centers using this method. Thus, the adequate estimation of TBSA is a primordial step in the appropriate management of the burn patient.
Detailed information regarding the IV fluid regimen administered at HIJG and given before transfer should be collected to enrich future research on this topic, and it would also increase knowledge on this matter a so all medical institutions may be able to standardize treatment in pediatric burn patients. Furthermore, the use of a mobile app such as e-burn was suggested to regional hospitals, although there was no tool to check its use in this study; this can also be considered in future research.
As published previously, in the large systematic review [23] published in 2021, present data show poor knowledge regarding burn injury estimation by non-specialists, creating the possibility to harm patients. Thus, it emerges the need of continued education and training in medical school, in order to upraise the quality of consults and be truthful to the duty of not causing harm, and, this way, avoiding one more variable that is likely to add to fluid creep.
Conclusion
The discrepancy between the evaluation of the TBSA before and after being transferred to the burn unit of HIJG proved to be outrageous, with overestimation in most cases (76.4% n=39), and represents a rough percentage of error within average 291% over the correct TBSA estimate.
This study also concluded that most (56.9% n=29) patients transferred to the burn unit of HIJG, in the state of Santa Catarina in southern Brazil, ranged in age from 1 to 4 years old. It also highlights that the main burn mechanism that injured those patients was hot water (scalding) that represented 60.8% of the sample. At last, it was shown that when fire and electric shock were responsible for the burn, the length of hospital stay was the longest; with in average 26 ± 9.3 days (p-value 0.014).
References
- Cruz BF, Cordovil PBL, Batista KNM. Perfil epidemiológico de pacientes que sofreram queimaduras no Brasil: revisão de literatura. Rev Bras Queimaduras. 2012; 11: 246-250.
- Ryan LM, Costabille P, Ziegfeld S, Puett L, Turner A, et al. Assessment of a quality improvement intervention to improve the consistency of total body surface area burn estimates between referring facilities and a pediatric burn center. Burns. 2019; 45: 1827-1832.
- Injury Data Visualization Tools | WISQARS | CDC. wisqars.cdc.gov. Available from: https://wisqars.cdc.gov/data/lcd/home. 2022.
- Dalla-Cortei, LM et al. Perfil epidemiológico de vítimas de queimaduras internadas em uma unidade no Distrito Federal do Brasil. Revista Brasileira de Queimaduras, Brasília. 2019; 18: 10-15.
- Secundo CO; Silva CCM; Feliszyn RS. Protocolo de cuidados de enfermagem ao paciente queimado na emergência: Revisão integrativa da literatura. Revista Brasileira de Queimaduras, Brasília. 2019; 18: 39-46.
- Mélega, JM. Cirurgia plástica os princípios e a atualidade. Rio de Janeiro Guanabara Koogan. 2011.
- Johnson, RM; Richard, Reg. Partial-Thickness Burns: identification and management. Identification and Management. Advances In Skin & Wound Care. 2003; 16: 178-187.
- JA Snell, Loh NHW, Mahambrey T, Shokrollahi K. Clinical review: the critical care management of the burn patient. : The critical care management of the burn patient. Critical Care, Liverpool, GB. 2013; 17: 241.
- Pham C, Collier Z, Gillenwater J. Changing the Way We Think About Burn Size Estimation. Journalof Burn Care & Research. 2018; 40: 1–11.
- Chong HP, Quinn L, Jeeves A, Cooksey R, Lodge M, Carney B, et al. A comparison study of methods for estimation of a burn surface area: Lund and Browder, e-burn and Mersey Burns. Burns. 2020; 46: 483–9.
- Daniels M, Fuchs PC, Lefering R, Grigutsch D, Seyhan H, Limper U, et al. Is the Parkland formula still the best method for determining the fluid resuscitation volume in adults for the first 24 hours after injury? — A retrospective analysis of burn patients in Germany. Burns. 2021; 47: 914-921.
- Yoda CN, Leonardi DF, Feijó R. Queimadura pediátrica: fatores associados a sequelas físicas em crianças queimadas atendidas no Hospital Infantil Joana de Gusmão. Rev Bras Queimaduras. 2013; 12: 112-117.
- AM Strobel, Fey R. Emergency Care of Pediatric Burns. Emergency Medicine Clinics of North America. 2018; 36: 441-458.
- Pisano C, Fabia R, Shi J, Wheeler K, Giles S, et al. Variation in acute fluid resuscitation among pediatric burn centers. Burns. 2021; 47: 545-550.
- Kramer GC, Lund T, Bechum O. Pathophysiology of burn shock and burn edema. In: David Herdron. Total Burn Care. Saunders Elsevier Philadelphia. 2007.
- Dittrich MHM, Hosni ND, de Carvalho WB. Association between fluid creep and infection in burned children: A cohort study. Burns. 2020; 46: 1036-1042.
- SBQ - Sociedade Brasileira de Queimaduras. www.sbqueimaduras. org.br. [cited 2022 May 30]. Availablefrom: http://www. sbqueimaduras.org.br/biblioteca-virtual
- Estimativas da população residente para os municípios e para as unidades da federação | IBGE. http://www.ibge.gov.br. [cited 2022 May 30] Available from: https://www.ibge.gov.br/estatisticas/ sociais/populacao/9103-estimativas-de- populacao. html?=&t=resultados.
- Ministério da Saúde (BR), Conselho Nacional de Saúde, Comissão Nacional de ética em Pesquisa. Resolução n 466 de 12 de dezembro de 2012: diretrizes e normas regulamentadoras de pesquisa envolvendo seres humanos. Brasília (DF): 2012.
- Ministério da Saúde (BR). Resolução nº 510, de 07 de abril de 2016. Dispõe sobre as normas aplicáveis a pesquisas em Ciências Humanas e Sociais. Diário Oficial [da] República Federativa do Brasil, Brasília, DF. 2016.
- Shah A, Pedraza I, Mitchell C, Kramer GC. Fluid volumes infused during burn resuscitation 1980–2015: A quantitative review. Burns. 2020; 46: 52–57.
- Armstrong JR, Willand L, Gonzalez B, Sandhu J, Mosier MJ. Quantitative Analysis of Estimated Burn Size Accuracy for Transfer Patients. Journal of Burn Care & Research. 2017; 38: e30–5.
- Brekke RL, Almeland SK, Hufthammer KO, Hansson E. Agreement of clinical assessment of burn size and burn depth between referring hospitals and burn centres: A systematic review. Burns. 2022: 00115-2.
- McCulloh C, Nordin A, Talbot LJ, Shi J, Fabia R, Thakkar RK. Accuracy of Prehospital Care Providers in Determining Total Body Surface Area Burned in Severe Pediatric Thermal Injury. Journal of Burn Care & Research. 2017; 39: 491–6.
- Harish V, Raymond AP, Issler AC, Lajevardi SS, Chang L-Y, Maitz PKM, et al. Accuracy of burn size estimation in patients transferred to adult Burn Units in Sydney, Australia: An audit of 698 patients. Burns. 2015; 41: 91–9.
- Partain KP, Fabia R, Thakkar RK. Pediatric burn care. Current Opinion in Pediatrics. 2020; 32: 405–10.
- Armstrong M, Wheeler KK, Shi J, Thakkar RK, Fabia RB, Groner JI, et al. Epidemiology and trend of US pediatric burn hospitalizations, 2003–2016. Burns. 2021; 47: 551–9.
- Purcell LN, Sincavage J, Banda W, Cairns B, Phillips MR, Gallaher JR, et al. The effect of burn mechanism on pediatric mortality in Malawi: A propensity weighted analysis. Burns. 2021; 47: 222–7.